Can’t see the audio player? Click here to download.
The Republican replacement proposal for the Affordable Care Act is moving forward in Congress, and major changes could be in store for millions of Californians.
House Republicans want to phase out the expansion of Medicaid starting in 2020. The program, known as Medi-Cal in California, has added nearly 4 million enrollees under the Obamacare expansion since 2014. The state also faces other potential cuts to Medi-Cal from a House plan for per-capita funding.
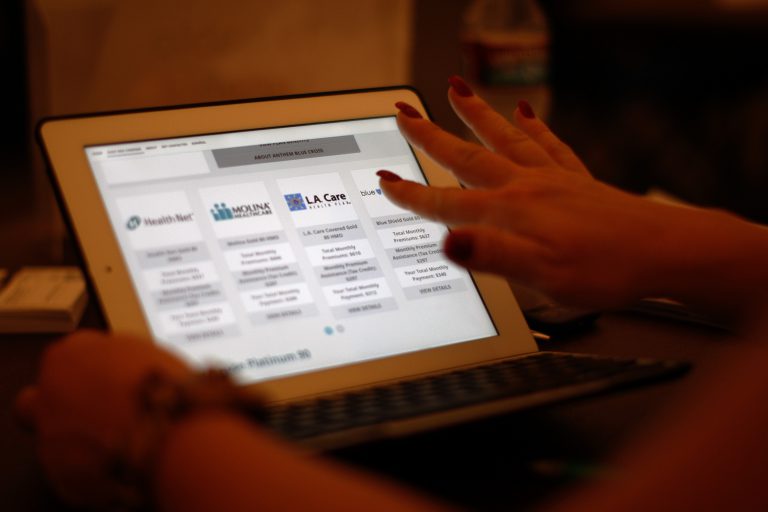
In the private insurance market, the House plan would dramatically alter the premium subsidies that about 1.2 million Californians receive to purchase coverage in the state exchange, Covered California. In many cases, lower-income and older consumers would receive less federal assistance under the GOP plan.
The Republican bill also ends the ACA’s individual mandate to have health insurance. In its place, people could face a 30 percent surcharge in premiums if they have a lapse in coverage.
Chad Terhune, a senior correspondent for California Healthline and Kaiser Health News, discussed the House bill and how it would work in California with A Martínez, host of the “Take Two” show on Southern California Public Radio (KPCC).