One of the few things that Republicans and Democrats broadly agree on is that states should have some flexibility to experiment with different ways to pay for and deliver health care.
But they disagree — strongly — on how much. In fact, Republicans don’t agree with one another on this, and that dissent helped sink efforts this summer to “repeal and replace” the Affordable Care Act. Bridging these divides will help determine the success of a bipartisan effort in the Senate this month to help shore up the individual health insurance market.
“I’ve always said not all the wisdom is going to be in Washington,” said Sen. Ron Wyden (D-Ore.), the ranking Democrat on the powerful Finance Committee. “Progressive and conservative folks are going to say ‘we can do better.’”
The federal health law includes a provision that allows states to alter some of its rules if they can think of a better way to provide health care to their residents. These are known as “Section 1332 waivers,” bookmarking where they are located in the health law.
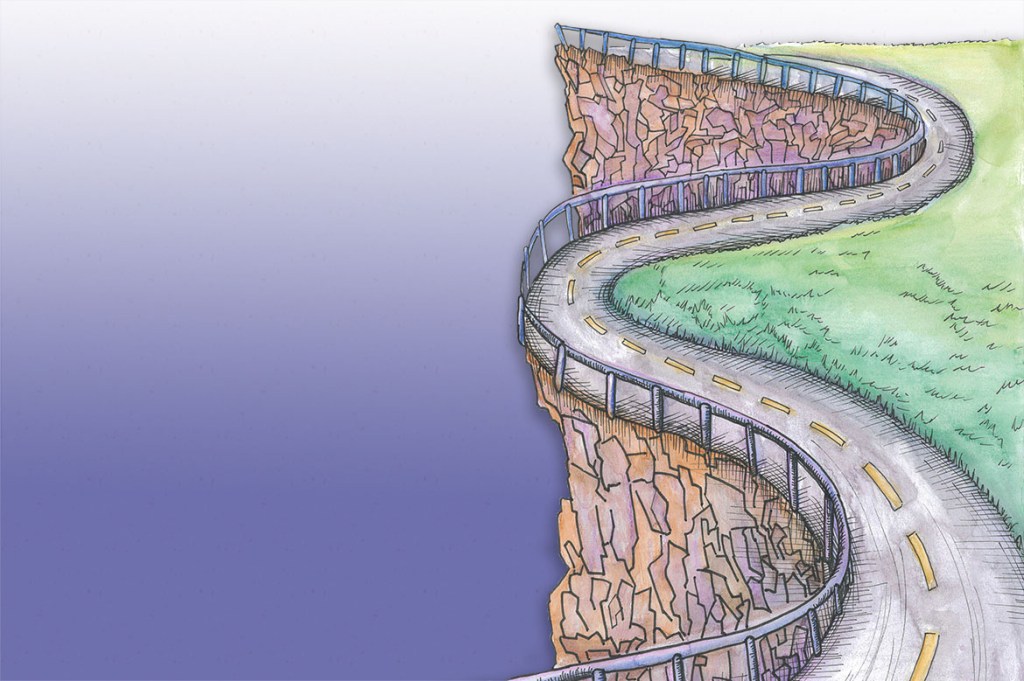
But the law strictly limits how far states can go with their experiments. It includes what are known as “guardrails.” Those limits, said Nicholas Bagley, a health law professor at the University of Michigan, “are to prevent states from undermining the Affordable Care Act goal to provide people with comprehensive coverage.”
The waivers were designed “so blue states can experiment with blue state solutions, and red states can experiment with red state solutions,” said Bagley. “But to do so and stay within the guardrails is really difficult.” For example, he said, “you can reallocate the money, but you can’t reallocate it to create losers.”
At issue is whether to broaden authority for states by revising or eliminating the “guardrails” intended to protect patients and the federal government.
Wyden, who authored the 1332 language in the ACA, is skeptical. Under the current rules, he said, “states can make changes that make health care better. But they can’t go out and make health care worse.”
It is clear that Republicans in Congress want changes to the provision. The repeal-and-replace bill that passed the House and all those considered in the Senate included some expansion of state authority to waive protections included in the health law. Bagley said the bills “would have essentially given carte blanche to states to come up with ACA alternatives without any regard to the guardrails” other than the one prohibiting additions to the federal deficit.
And Sen. Lamar Alexander (R-Tenn.), chairman of the Senate Health, Education, Labor and Pensions (HELP) Committee, who is working on a bipartisan bill, said Wednesday that “Democrats will have to agree to something — more flexibility for states — that some are reluctant to support.”
So is there a compromise between Democrats who want to maintain the protections and Republicans who want states to have a freer hand?
Maybe.
David Anderson of Duke University said one possible source of agreement would be to streamline the federal approval process, starting with the guidance issued by the Obama administration in 2015 that critics said was too restrictive.
Under the rules set by the ACA, states can use waivers to adjust things like the structure of premium assistance to those with low and moderate incomes or the individual and employer requirements to have and offer coverage. But those changes must meet four key standards: States continue to provide equally comprehensive coverage to at least the same number of people, with no higher out-of-pocket costs and without costing the federal government more than it would spend under the provisions of the ACA.
The rules around the waivers also make it hard to accomplish a truly comprehensive overhaul of a state’s health care system, as states can’t use them to reach the place where most of the money funding that system comes from: tax breaks for employer-provided insurance and the federal Medicare program. Workers don’t pay taxes on the value of employer-provided insurance, which is estimated to cost the federal Treasury some $260 billion in income and payroll taxes 2017.
“If you want to reshape your state health insurance market, you’ve got to be able to grab onto the employer market or Medicare, and you can’t” using the waiver procedure, Bagley said.
States also cannot use Section 1332 to change provisions of the Medicaid and Children’s Health Insurance Program, although they can submit simultaneous waivers to each program under separate Medicaid waiver authority in the law.
So far, only two states — Hawaii and Alaska — have won federal approval for 1332 waivers under the health law.
Hawaii has had its own system for providing health coverage based on an employer requirement for coverage since the 1970s. The state’s waiver allows it to use money allocated to help small businesses afford coverage in different ways.
Alaska’s waiver, which was approved this summer, involves a “reinsurance” plan that will help spread the costs of the state’s sickest patients more widely. “By removing high-cost conditions from the risk pool, the benefits of the [reinsurance program] are shared by the entire individual health insurance market,” Lori Wing-Heier, head of the state’s insurance department, told the HELP Committee on Wednesday. In its first year, the program dropped proposed premium increases from 40 percent to “just over 7 percent,” Wing-Heier said.
Minnesota has applied for a waiver similar to Alaska’s, and approval is expected. Earlier this spring, the Department of Health and Human Services specifically invited states to apply for waivers of that type.
Other states, though, are working on proposals that would make more comprehensive changes. Iowa, for example, wants to dramatically redistribute the money available, with bigger subsidies for the middle-class customers and smaller ones for those with lower incomes. The state says that would help draw more customers into the marketplace so that the risk pool is healthier and the premiums for everyone would decrease. It would also eliminate the help lower-income people get to pay their out-of-pocket medical costs, such as deductibles and copayments.
“The Iowa waiver on its face pretty brazenly ignores the guardrails,” said Bagley.
Oklahoma, which is seeking a waiver for its own reinsurance program, is also working on a plan that would make major changes, including encouraging people to purchase insurance with higher deductibles along with a health savings account.
Part of the difficulty with the waivers is the number of hoops states must jump through to win approval, including passing legislation, seeking public comment and holding hearings around the state.
And those are not even the biggest problems, state officials say. “The part that is stifling states right now is the six-month waiting period before they receive final approval,” Alaska’s Wing-Heier told the Senate panel.
Teresa Miller, former Pennsylvania insurance commissioner, agreed at the Senate hearing, saying, “The current process is very cumbersome.”
Anderson of Duke University said one key possibility to add flexibility would be to loosen the requirement that state changes not add to the federal deficit. “Maybe they could allow for deficit neutrality over the course of the waiver rather than year by year,” he said, in which case experiments that cost money to begin with but save over time would be allowed.
Wyden said he is willing to look at any ideas to make the waivers easier to use.
But he added that the popularity of state “reinsurance” waivers that are lowering premiums shows the waiver provision is working as intended. And, he said, if GOP members try again to roll back coverage using the waiver provision “they’re going to have to roll over me, then they’re going to have to persuade people” that it meets the 1332 requirements.
This story was produced by Kaiser Health News, an editorially independent program of the Kaiser Family Foundation.