Workers at Garfield Medical Center in suburban Los Angeles were on edge as the pandemic ramped up in March and April. Staffers in a 30-patient unit were rationing a single tub of sanitizing wipes all day. A May memo from the CEO said N95 masks could be cleaned up to 20 times before replacement.
Patients showed up COVID-negative but some still developed symptoms a few days later. Contact tracing took the form of texts and whispers about exposures.
By summer, frustration gave way to fear. At least 60 staff members at the 210-bed community hospital caught COVID-19, according to records obtained by KHN and interviews with eight staff members and others familiar with hospital operations.
The first to die was Dawei Liang, 60, a quiet radiology technician who never said no when a colleague needed help. A cardiology technician became infected and changed his final wishes — agreeing to intubation — hoping for more years to dote on his grandchildren.
Few felt safe.
Ten months into the pandemic, it has become far clearer why tens of thousands of health care workers have been infected by the virus and why so many have died: dire PPE shortages. Limited COVID tests. Sparse tracking of viral spread. Layers of flawed policies handed down by health care executives and politicians, and lax enforcement by government regulators.
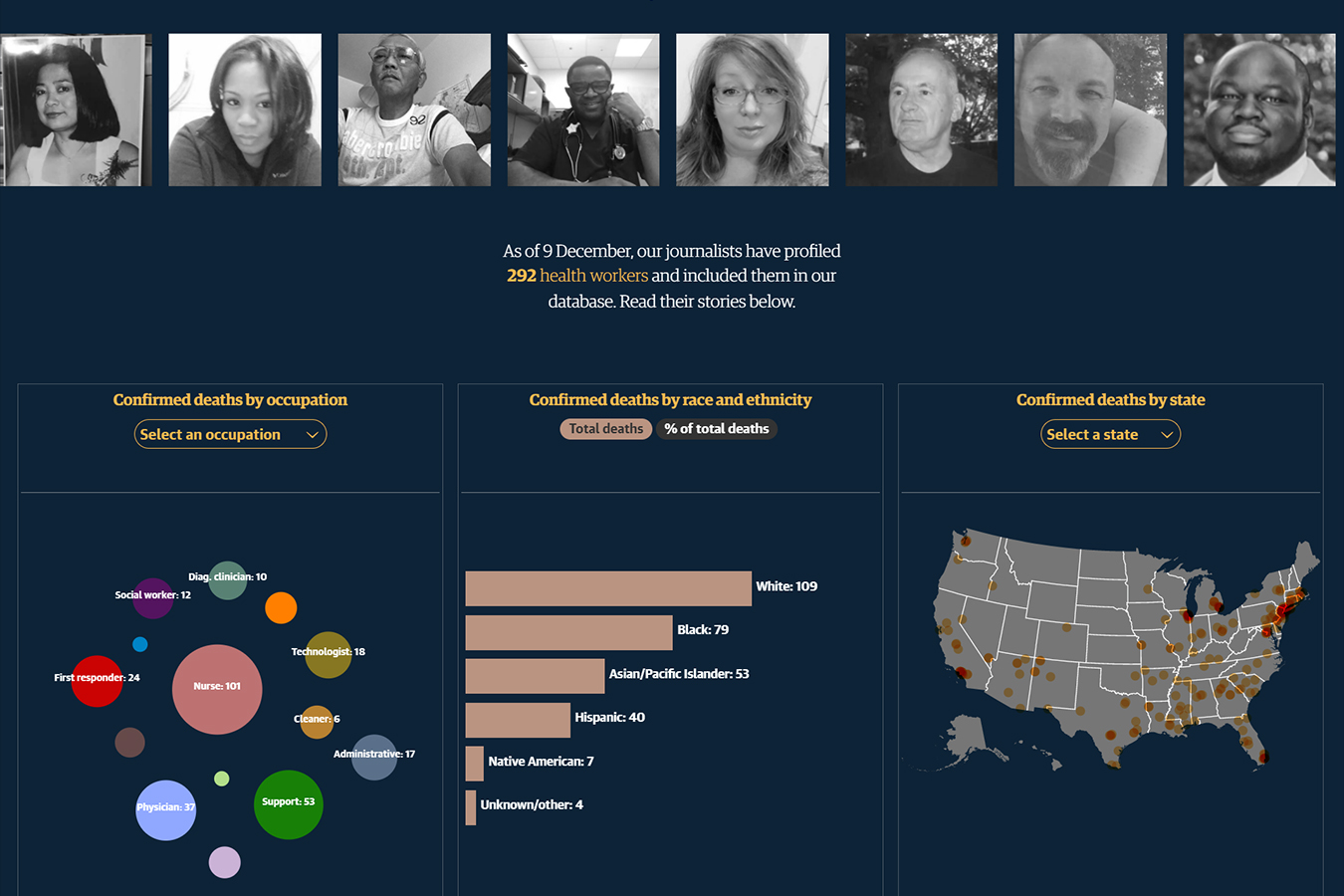
All of those breakdowns, across cities and states, have contributed to the deaths of more than 2,900 health care workers, a nine-month investigation by over 70 reporters at KHN and The Guardian has found. This number is far higher than that reported by the U.S. government, which does not have a comprehensive national count of health care workers who’ve died of COVID-19.
Explore The Database
KHN and The Guardian are tracking health care workers who died from COVID-19 and writing about their lives and what happened in their final days.
Read Their StoriesThe fatalities have skewed young, with the majority of victims under age 60 in the cases for which there is age data. People of color have been disproportionately affected, accounting for about 65% of deaths in cases in which there is race and ethnicity data. After conducting interviews with relatives and friends of around 300 victims, KHN and The Guardian learned that one-third of the fatalities involved concerns over inadequate personal protective equipment.
Many of the deaths occurred in New York and New Jersey, and significant numbers also died in Southern and Western states as the pandemic wore on.
Workers at well-funded academic medical centers — hubs of policymaking clout and prestigious research — were largely spared. Those who died tended to work in less prestigious community hospitals like Garfield, nursing homes and other health centers in roles in which access to critical information was low and patient contact was high.
Garfield Medical Center and its parent company, AHMC Healthcare, did not respond to multiple calls or emails regarding workers’ concerns and circumstances leading to the worker deaths.
So as 2020 draws to a close, we ask: Did so many of the nation’s health care workers have to die?
New York’s Warning for the Nation
The seeds of the crisis can be found in New York and the surrounding cities and suburbs. It was the region where the profound risks facing medical staff became clear. And it was here where the most died.
In COVID Hot Zones, Firefighters Now ‘Pump More Oxygen Than Water’
Firefighters are often thrust into front-line health emergencies. During the COVID pandemic, they’ve paid an especially high price.
Read MoreAs the pandemic began its U.S. surge, city paramedics were out in force, their sirens cutting through eerily empty streets as they rushed patients to hospitals. Carlos Lizcano, a blunt Queens native who had been with the New York City Fire Department (FDNY) for two decades, was one of them.
He was answering four to five cardiac arrest calls every shift. Normally he would have fielded that many in a month. He remembered being stretched so thin he had to enlist a dying man’s son to help with CPR. On another call, he did chest compressions on a 33-year-old woman as her two small children stood in the doorway of a small apartment.
“I just have this memory of those kids looking at us like, ‘What’s going on?’”
After the young woman died, Lizcano went outside and punched the ambulance in frustration and grief.
The personal risks paramedics faced were also grave.
More than 40% of emergency medical service workers in the FDNY went on leave for confirmed or suspected coronavirus during the first three months of the pandemic, according to a study by the department’s chief medical officer and others.
In fact, health care workers were three times more likely than the general public to get COVID-19, other researchers found. And the risks were not equally spread among medical professions. Initially, CDC guidelines were written to afford the highest protection to workers in a hospital’s COVID-19 unit.
Yet months later, it was clear that the doctors initially thought to be at most risk — anesthesiologists and those working in the intensive care unit — were among the least likely to die. This could be due to better personal protective equipment or patients being less infectious by the time they reach the ICU.
Instead, scientists discovered that “front door” health workers like paramedics and those in acute-care “receiving” roles — such as in the emergency room — were twice as likely as other health care workers to be hospitalized with COVID-19.
For FDNY’s first responders, part of the problem was having to ration and reuse masks. Workers were blind to an invisible threat that would be recognized months later: The virus spread rapidly from pre-symptomatic people and among those with no symptoms at all.
In mid-March, Lizcano was one of thousands of FDNY first responders infected with COVID-19.
At least four of them died, city records show. They were among the 679 health care workers who have died in New York and New Jersey to date, most at the height of the terrible first wave of the virus.
“Initially, we didn’t think it was this bad,” Lizcano said, recalling the confusion and chaos of the early pandemic. “This city wasn’t prepared.”
Neither was the rest of the country.
An Elusive Enemy
The virus continued to spread like a ghost through the nation and proved deadly to workers who were among the first to encounter sick patients in their hospital or nursing home. One government agency had a unique vantage point into the problem but did little to use its power to cite employers — or speak out about the hazards.
Health employers had a mandate to report worker deaths and hospitalizations to the Occupational Safety and Health Administration.
When they did so, the report went to an agency headed by Eugene Scalia, son of conservative Supreme Court Justice Antonin Scalia who died in 2016. The younger Scalia had spent part of his career as a corporate lawyer fighting the very agency he was charged with leading.
OSHA Let Employers Decide Whether to Report Health Care Worker Deaths. Many Didn’t.
Four workers died at a facility with one of the largest U.S. outbreaks, but the Occupational Safety and Health Administration never conducted an inspection. It’s a pattern that’s played out across the nation, a KHN investigation finds.
Read MoreIts inspectors have documented instances in which some of the most vulnerable workers — those with low information and high patient contact — faced incredible hazards, but OSHA’s staff did little to hold employers to account.
Beaumont, Texas, a town near the Louisiana border, was largely untouched by the pandemic in early April.
That’s when a 56-year-old physical therapy assistant at Christus Health’s St. Elizabeth Hospital named Danny Marks called in sick with a fever and body aches, federal OSHA records show.
He told a human resources employee that he’d been in the room of a patient who was receiving a breathing treatment — the type known as the most hazardous to health workers. The CDC advises that N95 respirators be used by all in the room for the so-called aerosol-generating procedures. (A facility spokesperson said the patient was not known or suspected to have COVID at the time Marks entered the room.)
Marks went home to self-isolate. By April 17, he was dead.
The patient whose room Marks entered later tested positive for COVID-19. And an OSHA investigation into Marks’ death found there was no sign on the door to warn him that a potentially infected patient was inside, nor was there a cart outside the room where he could grab protective gear.
The facility did not have a universal masking policy in effect when Marks went in the room, and it was more than likely that he was not wearing any respiratory protection, according to a copy of the report obtained through a public records request. Twenty-one more employees contracted COVID by the time he died.
“He was a beloved gentleman and friend and he is missed very much,” Katy Kiser, Christus’ public relations director, told KHN.
Tell Us A Health Worker’s Story
Do you know of a colleague or loved one who should be included in the “Lost On The Frontline” series? Please share their story.
Submit A NameOSHA did not issue a citation to the facility, instead recommending safety changes.
The agency logged nearly 8,700 complaints from health care workers in 2020. Yet Harvard researchers found that some of those desperate pleas for help, often decrying shortages of PPE, did little to forestall harm. In fact, they concluded that surges in those complaints preceded increases in deaths among working-age adults 16 days later.
One report author, Peg Seminario, blasted OSHA for failing to use its power to get employers’ attention about the danger facing health workers. She said issuing big fines in high-profile cases can have a broad impact — except OSHA has not done so.
“There’s no accountability for failing to protect workers from exposure to this deadly virus,” said Seminario, a former union health and safety official.
Desperate for Safety Gear
There was little outward sign this summer that Garfield Medical Center was struggling to contain COVID-19. While Medicare has forced nursing homes to report staff infections and deaths, no such requirement applies to hospitals.
Yet as the focus of the pandemic moved from the East Coast in the spring to Southern and Western states, health care worker deaths climbed. And behind the scenes at Garfield, workers were dealing with a lack of equipment meant to keep them safe.
Complaints to state worker-safety officials filed in March and April said Garfield Medical Center workers were asked to reuse the same N95 respirator for a week. Another complaint said workers ran out of medical gowns and were directed to use less-protective gowns typically provided to patients.
Staffers were shaken by the death of Dawei Liang. And only after his death and a rash of infections did Garfield provide N95 masks to more workers and put up plastic tarps to block a COVID unit from an adjacent ward. Yet this may have been too late.
The coronavirus can easily spread to every corner of a hospital. Researchers in South Africa traced a single ER patient to 119 cases in a hospital — 80 among staff members. Those included 62 nurses from neurology, surgical and general medical units that typically would not have housed COVID patients.
By late July, Garfield cardiac and respiratory technician Thong Nguyen, 73, learned he was COVID-positive days after he collapsed at work. Nguyen loved his job and was typically not one to complain, said his youngest daughter, Dinh Kozuki. A 34-year veteran at the hospital, he was known for conducting medical tests in multiple languages. His colleagues teased him, saying he was never going to retire.
Kozuki said her father spoke up in March about the rationing of protective gear, but his concerns were not allayed.

The PPE problems at Garfield were a symptom of a broader problem. As the virus spread around the nation, chronic shortages of protective gear left many workers in community-based settings fatally exposed. Nearly 1 in 3 family members or friends of around 300 health care workers interviewed by KHN or The Guardian expressed concerns about a fallen workers’ PPE.
Health care workers’ labor unions asked for the more-protective N95 respirators when the pandemic began. But Centers for Disease Control and Prevention guidelines said the unfitted surgical masks worn by workers who feed, bathe and lift COVID patients were adequate amid supply shortages.
Mary Turner, an ICU nurse and president of the Minnesota Nurses Association, said she protested alongside nurses all summer demanding better protective gear, which she said was often kept from workers because of supply-chain shortages and the lack of political will to address them.
“It shouldn’t have to be that way,” Turner said. “We shouldn’t have to beg on the streets for protection during a pandemic.”
At Garfield, it was even hard to get tested. Critical care technician Tony Ramirez said he started feeling ill on July 12. He had an idea of how he might have been exposed: He’d cleaned up urine and feces of a patient suspected of having COVID-19 and worked alongside two staffers who also turned out to be COVID-positive. At the time, he’d been wearing a surgical mask and was worried it didn’t protect him.
Yet he was denied a free test at the hospital, and went on his own time to Dodger Stadium to get one. His positive result came back a few days later.
As Ramirez rested at home, he texted Alex Palomo, 44, a Garfield medical secretary who was also at home with COVID-19, to see how he was doing. Palomo was the kind of man who came to many family parties but would often slip away unseen. A cousin finally asked him about it: Palomo said he just hated to say goodbye.
Palomo would wear only a surgical mask when he would go into the rooms of patients with flashing call lights, chat with them and maybe bring them a refill of water, Ramirez said.

Ramirez said Palomo had no access to patient charts, so he would not have known which patients had COVID-19: “In essence, he was helping blindly.”
Palomo never answered the text. He died of COVID-19 on Aug. 14.
And Thong Nguyen had fared no better. His daughter, a hospital pharmacist in Fresno, had pressed him to go on a ventilator after seeing other patients survive with the treatment. It might mean he could retire and watch his grandkids grow up. But it made no difference.
“He definitely should not have passed [away],” Kozuki said.
Nursing Homes Devastated
During the summer, as nursing homes recovered from their spring surge, Heather Pagano got a new assignment. The Doctors Without Borders adviser on humanitarianism had been working in cholera clinics in Nigeria. In May, she arrived in southeastern Michigan to train nursing home staffers on optimal infection-control techniques.
Federal officials required worker death reports from nursing homes, which by December tallied more than 1,100 fatalities. Researchers in Minnesota found particular hazards for these health workers, concluding they were the ones most at risk of getting COVID-19.
Pagano learned that staffers were repurposing trash bin liners and going to the local Sherwin-Williams store for painting coveralls to backfill shortages of medical gowns. The least-trained clinical workers — nursing assistants — were doing the most hazardous jobs, turning and cleaning patients, and brushing their teeth.
Hospitals, Nursing Homes Fail to Separate COVID Patients, Putting Others at Risk
COVID patients have been commingled with uninfected patients in California, Florida, New Jersey, Iowa, Ohio, Maryland, New York and beyond. While officials have penalized nursing homes for such failures, hospitals have seen less scrutiny.
Read MoreShe said nursing home leaders were shuffling reams of federal, state and local guidelines yet had little understanding of how to stop the virus from spreading.
“No one sent trainers to show people what to do, practically speaking,” she said.
As the pandemic wore on, nursing homes reported staff shortages getting worse by the week: Few wanted to put their lives on the line for $13 an hour, the wage for nursing assistants in many parts of the U.S.
The organization GetusPPE, formed by doctors to address shortages, saw almost all requests for help were coming from nursing homes, doctors’ offices and other non-hospital facilities. Only 12% of the requests could be fulfilled, its October report said.
And a pandemic-weary and science-wary public has fueled the virus’s spread. In fact, whether or not a nursing home was properly staffed played only a small role in determining its susceptibility to a lethal outbreak, University of Chicago public health professor Tamara Konetzka found. The crucial factor was whether there was widespread viral transmission in the surrounding community.
“In the end, the story has pretty much stayed the same,” Konetzka said. “Nursing homes in virus hot spots are at high risk and there’s very little they can do to keep the virus out.”
The Vaccine Arrives
From March through November, 40 complaints were filed about the Garfield Medical Center with the California Department of Public Health, nearly three times the statewide average for the time. State officials substantiated 11 complaints and said they are part of an ongoing inspection.
For Thanksgiving, AHMC Healthcare Chairman Jonathan Wu sent hospital staffers a letter thanking “frontline healthcare workers who continue to serve, selflessly exposing themselves to the virus so that others may cope, recover and survive.”
The letter made no mention of the workers who had died. “A lot of people were upset by that,” said critical care technician Melissa Ennis. “I was upset.”
By December, all workers were required to wear an N95 respirator in every corner of the hospital, she said. Ennis said she felt unnerved taking it off. She took breaks to eat and drink in her car.
Garfield said on its website that it is screening patients for the virus and will “implement infection prevention and control practices to protect our patients, visitors, and staff.”
On Dec. 9, Ennis received notice that the vaccine was on its way to Garfield. Nationwide, the vaccine brought health workers relief from months of tension. Nurses and doctors posted photos of themselves weeping and holding their small children.
At the same time, it proved too late for some. A new surge of deaths drove the toll among health workers to more than 2,900.
And before Ennis could get the shot, she learned she would have to wait at least a few more days, until she could get a COVID test.
She found out she’d been exposed to the virus by a colleague.
Video by Hannah Norman
Web production by Lydia Zuraw
This story is part of “Lost on the Frontline,” an ongoing project from The Guardian and Kaiser Health News that aims to document the lives of health care workers in the U.S. who die from COVID-19, and to investigate why so many are victims of the disease. If you have a colleague or loved one we should include, please share their story.
This story was produced by KHN (Kaiser Health News), a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.