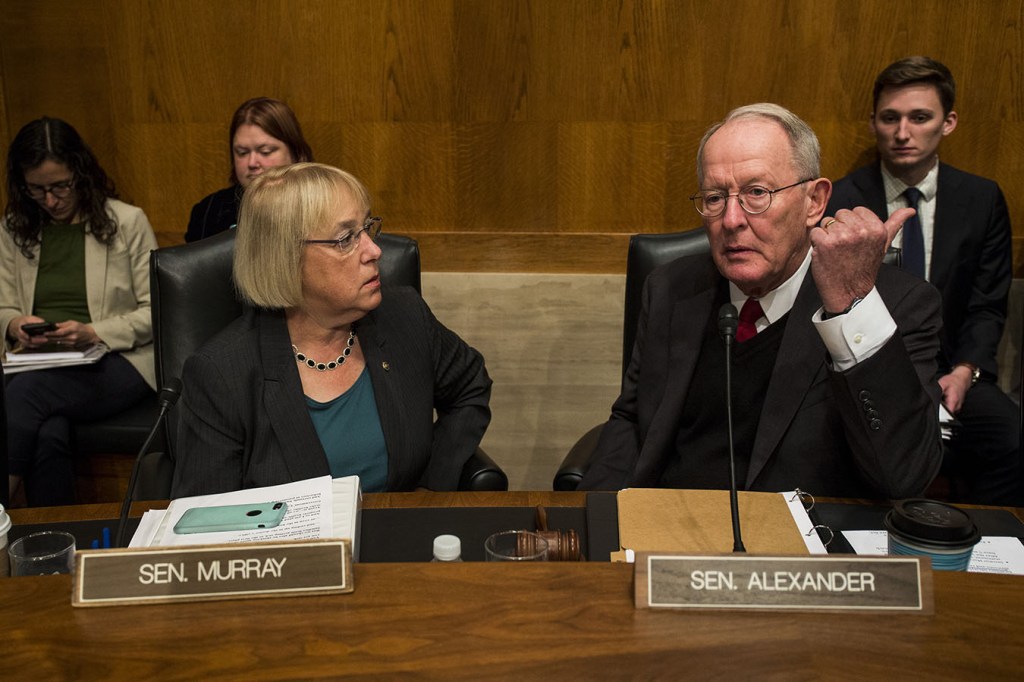
In a year already marked by a wide variety of congressional health care legislation, Sens. Lamar Alexander (R-Tenn.) and Patty Murray (D-Wash.), the chair and ranking Democrat of the Health, Education, Labor and Pensions Committee, on Thursday released the details of a plan they hope can help bring down health costs and eliminate surprise medical bills for patients.
“These are common sense steps we can take, and every single one of them has the objective of reducing the health care costs that you pay for out of your own pocket,” Alexander said in a statement. “We hope to move it through the health committee in June, put it on the Senate floor in July and make it law.”
It would be a mammoth piece of legislation, targeting nearly every area of the health care industry for reform, including surprise medical bills, prescription drugs, transparency, public health and health information. Alexander said at a White House event earlier this month that he hopes to get the package to the Senate floor by the end of July.
“When you have a chairman and a ranking member that have worked together on a bipartisan package in the committee of jurisdiction, it always gives more weight to the product,” said Dean Rosen a former Republican senior health adviser and a partner at Mehlman Castagnetti Rosen & Thomas.
“Folks should take this package seriously,” he added.
The draft bill released by the senators offers three options to curb surprise bills, those unexpected and often pricey bills patients face when they get care from a doctor or hospital that isn’t in their insurance network. It would use an independent arbitrator to settle disputes between insurance plans and providers and set a standard benchmark for physician pay, ideas that have popped up in other draft legislation circulating in the House and Senate.
The novel part from Alexander and Murray is the idea of an “in-network guarantee.” It requires that any hospital considered “in-network” for a health plan must promise that everyone working there is also in-network.
This would avoid situations in which patients choose a hospital because they know their insurance company will cover the bill, only to find out that one of the doctors they saw was out-of-network, leaving the patient with a hefty bill.
It also requires that labs and diagnostic tests be in-network, cutting off another avenue of surprise bills.
“From a policy perspective, there’s a rationale that this is the ideal approach,” said Loren Adler, the associate director of USC-Brookings Schaeffer Initiative for Health Policy.
Often called “network matching,” it’s an approach championed by the health insurance industry. James Gelfand, senior vice president for health policy for the ERISA Industry Committee, named it specifically as a solution during testimony at a surprise bill hearing in the House Ways and Means Committee on Tuesday. Rep. Lloyd Doggett (D-Texas) has suggested something similar in bills introduced in this session and two past congresses.
It’s possible that this option will upset provider groups, who risk receiving lower payments and having less leverage with insurance companies. Adler said these fears are mostly unfounded because hospitals have a vested interest in being fully staffed; they’ll step in if insurance companies try to lowball doctors.
Stakeholders such as industry trade groups, lobbyists and consultants will get a chance to air those concerns at a closed briefing on the draft on Capitol Hill Thursday.
The Alexander-Murray proposal joins an array of efforts on surprise billing. The White House held an event featuring patients, several House committees have held hearings, and bipartisan groups in the House and Senate have proposed legislation, including a bill from Sens. Bill Cassidy (R-La.) and Maggie Hassan (D-N.H.). In addition to Alexander and Murray’s proposal, the details of another bipartisan bill were released Thursday from Rep. Raul Ruiz (D-Calif.) and Rep. Phil Roe (R-Tenn.), both also physicians.
But Alexander and Murray’s proposal also covers a wide array of issues, and it’s not clear how that will play in Congress just a few months from the start of a presidential election season.
“The steps we are taking on important issues like surprise medical billing, drug prices, maternal mortality, and vaccine hesitancy show we can make progress when both sides are at the table ready to put patients and families first,” said Murray.
“I think it is an ambitious package,” Rosen said. “I think it’s probably going to be a challenge to get all of this done.”
The Alexander-Murray proposal also tackles prescription drug pricing reform, another issue that has raised bipartisan concerns and spurred hearings across the Capitol this spring.
Instead of regulating drug prices, the package would address patent protections, making it easier for generics to get to market and harder for brand-name drugs to maintain exclusive patents for lengthy periods.
It also addresses pharmacy benefit managers, which have lately come under scrutiny in the drug pricing debate. PBMs act as middlemen between drugmakers and insurance plans to negotiate prices and have been blamed by some in the pharmaceutical industry for keeping medication costs high.
The proposal suggests requiring PBMs to give quarterly reports on costs, fees and information about rebates — which are the discounts drugmakers offer to PBMs in exchange for making sure their medication is covered under a health plan. The bill also requires that 100% of these discounts be passed on to consumers.
Other provisions include requiring health plans and providers to give patients estimates of out-of-pocket-costs for a service within 48 hours of a request and mandating that medical bills be sent within 30 days of a procedure.
The bill addresses a host of other health-related issues, including some making headlines recently:
- Money for programs to educate people about vaccines and programs to reduce vaccine-preventable diseases.
- Grants to study and improve maternal mortality and improve pregnancy and postpartum care.
- Money for better training for health care professionals to prevent discrimination and bias.
- Measures to improve privacy and cybersecurity for health information and electronic medical records.
This story was produced by Kaiser Health News, an editorially independent program of the Kaiser Family Foundation.