Hospital systems and health officials have been calling urgently for more primary care doctors, but graduates of U.S. medical schools are becoming less likely to specialize in one of the primary care fields.
That’s a problem, because experts predict the U.S. will experience a significant primary care physician shortage in the next thirteen years. In California alone, a shortfall of 4,700 primary care doctors is projected by 2025.
Some medical schools in the Golden State are striving to address the expected shortage.
The University of California-Riverside School of Medicine has emphasized primary care training since its first class enrolled in 2013. This year, about 60% of the school’s graduates chose primary care specialties. The Keck Graduate Institute, which announced last year it is opening a school of medicine in Southern California, will focus on training its students to become primary care physicians in the region.
And Kaiser Permanente’s new medical school in Pasadena, Calif., which will enroll its first class in the summer of 2020, is offering incentives to make primary care more financially appealing to students interested in pursuing it. (Kaiser Health News, which produces California Healthline, is not affiliated with Kaiser Permanente.)
Across the U.S., a record-high number of primary care positions was offered in the 2019 National Resident Matching Program — known to doctors as “the Match” – which determines the specialty a medical student will study after graduation. But this year, the percentage of primary care positions filled by fourth-year medical students was the lowest on record.
“I think part of it has to do with income,” said Mona Signer, the CEO of the Match. “Primary care specialties are not the highest paying.” She suggested that where a student gets a degree also influences the choice. “Many medical schools are part of academic medical centers where research and specialization is a priority,” she said.
The three key primary care fields are internal medicine, family medicine and pediatrics. According to the 2019 Match report, 8,116 internal medicine positions were offered, the highest number on record and the most among any specialty. Only 41.5% of those positions were filled by seniors pursuing their M.D.s at U.S. medical schools. Similar trends were seen this year in family medicine and pediatrics.
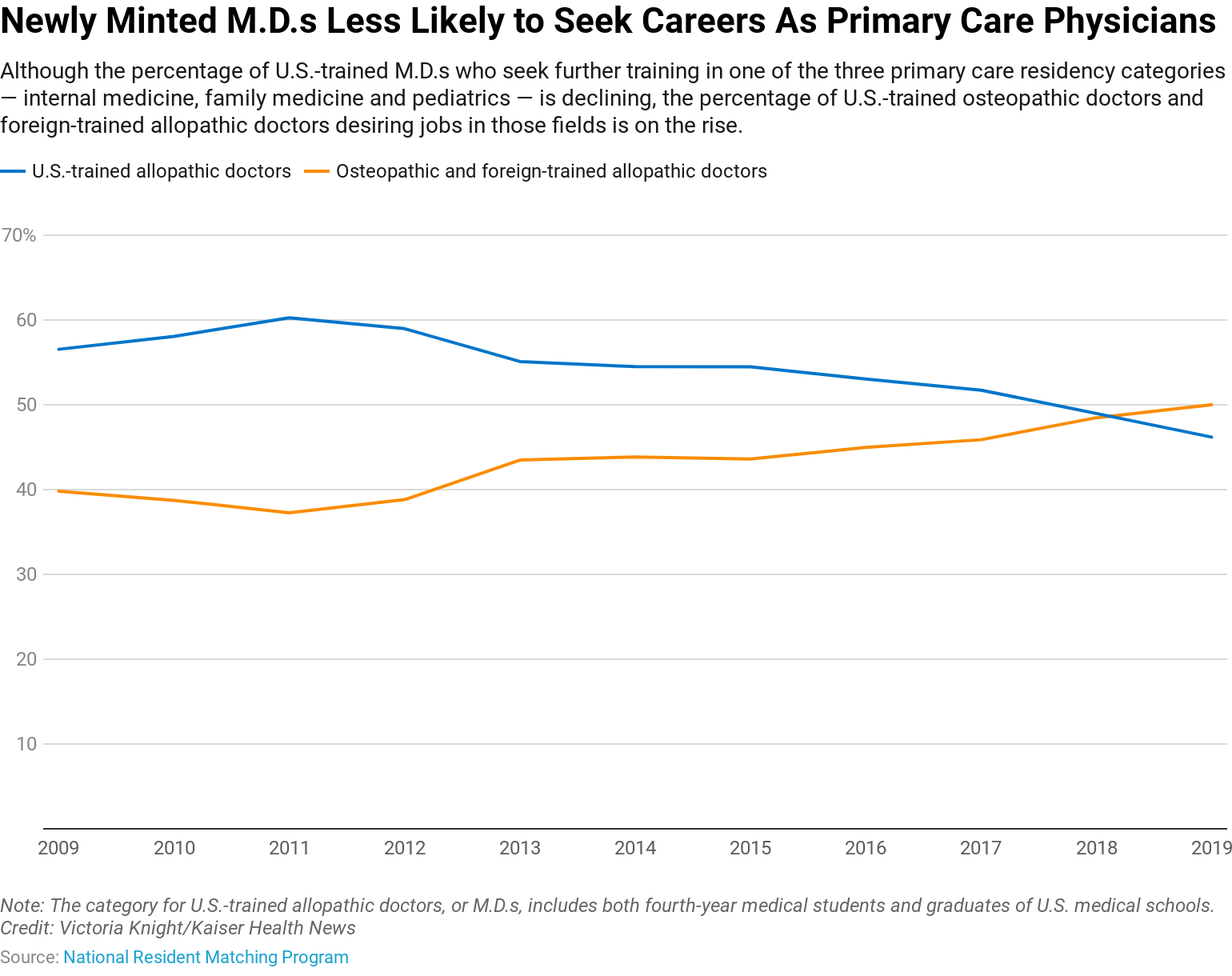
Since 2011, the percentage of U.S.-trained allopathic or M.D. physicians who have matched into primary care positions has declined, according to an analysis of historical Match data by Kaiser Health News.
Over the same period, the percentage of U.S.-trained osteopathic and foreign-trained physicians selecting primary care roles has increased. This is the first year in which the percentage of osteopathic and foreign-trained doctors exceeds the percentage of U.S. trained medical doctors taking primary care positions.’
The five medical schools with the highest percentage of graduates who chose primary care are all osteopathic institutions, according to the latest U.S. News & World Report survey.
Physicians who are trained at foreign medical schools, including both U.S. and non-U.S. citizens, also take unfilled primary care residency positions. In the 2019 match, 68.9% of foreign-trained physicians went into internal medicine, family medicine and pediatrics.
But, despite osteopathic graduates and foreign-trained medical doctors taking up these primary care spots, a primary care physician shortage is still expected as more doctors are needed in the coming years to care for aging baby boomers, many of whom have multiple chronic conditions.
Studies have shown that states with a higher ratio of primary care physicians have better health and lower rates of mortality. Patients who regularly see a primary care physician also have lower health costs than those without one.
But choosing a specialty other than primary care often means a higher paycheck.
According to a recently published survey of physicians conducted by Medscape, internal medicine doctors’ salaries average $243,000 annually. That’s a little over half of what the highest earners, orthopedic physicians, make with an average annual salary of $482,000. Family medicine and pediatrics earn even less than internal medicine, at $231,000 and $225,000 per year, respectively.
Dr. Eric Hsieh, the internal medicine residency program director for the University of Southern California’s Keck School of Medicine, said that when he chose his specialty he consciously accepted the lower pay because he liked the idea of developing an ongoing relationship with patients.
“There’s a lot of other fields where you can swoop in and fix the problem and then leave,” Hsieh said. “But a lot of primary care is getting to know a person. It doesn’t happen with one or two meetings, you need to have a relationship, talk to them about their families and hobbies. That’s how you then build an individualized plan that helps to make them healthier.”
He acknowledged that a possible deterrent to choosing internal medicine is the amount of time required to fill out patients’ electronic medical records. The Medscape survey confirms that internists appear to be more burdened with paperwork than other specialties: 80% of them reported spending 10 or more hours per week on administrative tasks. The result: Only 62% of internal medicine doctors said they would choose to go into their specialty again — the lowest percentage on record for all physician specialties surveyed.
Elsa Pearson, a health policy analyst at Boston University, said another solution should be shifting some primary care tasks to health care providers who aren’t doctors, such as nurse practitioners or physician assistants.
And spreading the word about loan forgiveness programs available to young primary care doctors who agree to work in underserved areas of the country can also help, said Dr. Tyree Winters, the associate director of the pediatric residency program at Goryeb Children’s Hospital in New Jersey.
Kaiser Permanente’s medical school has said it will waive tuition for its first five classes.
“What we want to do is create a situation where students can follow their dreams without taking debt into account,” Dr. Mark Schuster, the school’s founding dean and CEO, told KHN. “For those who want to pursue primary care or serve underserved communities, we hope this will let them feel free to do that.”
Kaiser Health News data correspondent Sydney Lupkin contributed to this report.
This story was produced by Kaiser Health News, an editorially independent program of the Kaiser Family Foundation.


