Even as U.S. authorities have taken the drastic steps of quarantining residents returning from China, and temporarily banning foreign visitors who recently traveled to affected Chinese regions, they have urged the vast majority of U.S. residents to go about their regular activities.
But there are exceptions. People who returned from China on or after Feb. 3 have been formally quarantined or asked to stay home. And behind the scenes, local public health officials have launched painstaking efforts to reach “close contacts” of people with confirmed cases of the virus, dubbed 2019-nCoV, asking them to self-quarantine and submit to ongoing monitoring.
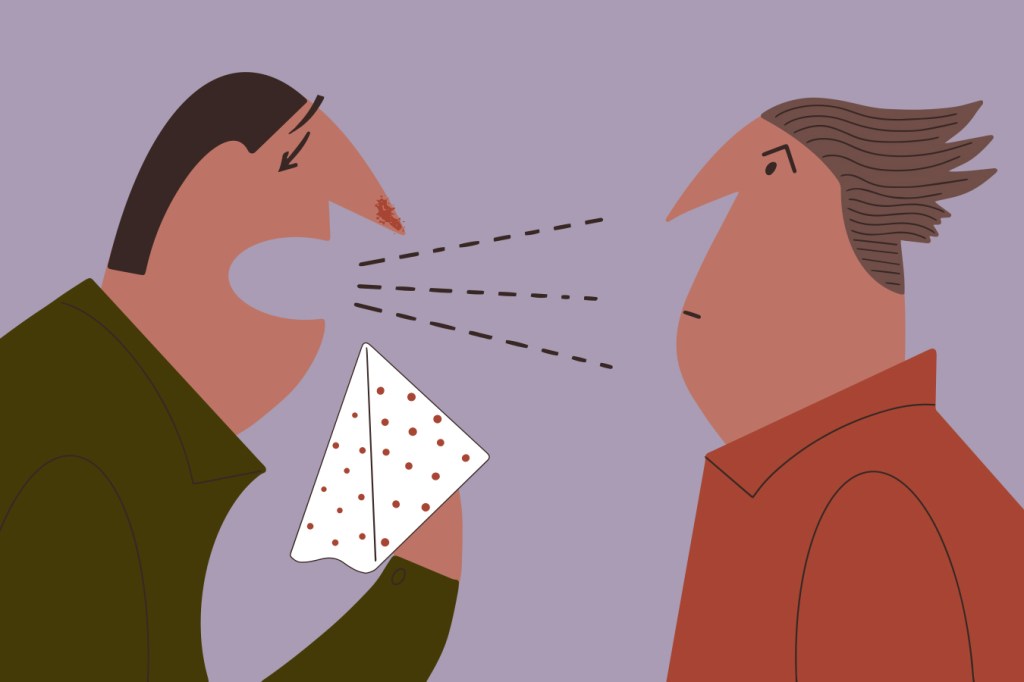
So what exactly is a “close contact”? It’s an intuitive-sounding term, but has a clinical definition that varies by infectious disease. The deadly measles virus, for example, can linger in a place for hours, in the air and on surfaces, after an infected person has spent time there. Coronaviruses are generally passed through droplets, requiring close physical contact with a sneeze or other body secretion.
How a virus is spread, and the severity of the illness it causes, determines how public health departments decide how many people are at risk of contagion and how many resources go into notifying them. When it comes to measles, officials broadly publicize every known location an infected person frequented in the days before being diagnosed, and try to track down people who came in contact with that patient who have not been vaccinated. For the new coronavirus, guidelines from the federal Centers for Disease Control and Prevention define “close contact” as anyone who has been within 6 feet of a person infected with the virus for a “prolonged period of time,” as well as those who have had direct contact with the infected person’s secretions. These guidelines are then interpreted by local public health departments.
The European Union’s health agency offers a descriptive definition: someone living in the same household as a patient; someone who has had face-to-face contact with or been in a closed environment with a patient; or a health care worker directly caring for a patient. It’s also any plane (and by extension, train or bus) passenger sitting within two seats, in any direction, of an infected person. The World Health Organization flags health care providers and household members, as well as anyone who has been within 3 feet of a confirmed case once the infected person had symptoms.
Translating those guidelines to real people and their daily movements is at the heart of what public health departments around the country do for any infectious disease. Local investigators work with patients to find out where they were and what they did in the days before they were diagnosed. They identify anyone who might be at risk for infection, track them down and help monitor their health. Depending on how close the contact was, health officials may ask the contact to temporarily stay away from others.
As of Monday, tens of thousands of people in mainland China were confirmed to have the disease, and hundreds had died. But in the U.S, there have been just a dozen cases so far, nearly all among people who recently returned from the country of 1.4 billion. State and federal health officials stress that the risk of getting the virus in this country remains low.
Santa Clara County in California has reported two confirmed cases of the virus, both in people who recently traveled to China. Anyone who lived with one of those people would be considered at high risk, said Dr. Sarah Rudman, an assistant public health officer with the county. They are monitored for symptoms, and asked to stay home and away from others for two weeks. To date, the only two people known to have caught the virus via human-to-human transmission in the U.S. live with someone who got it in China.
Health care workers also are given special consideration. Li Wenliang, a 34-year-old doctor in Wuhan, China, where the outbreak began, raised early alarm bells about the virus after several cases appeared in the hospital where he worked. He ultimately contracted the illness and died on Feb. 6, according to hospital officials. Multiple other health care workers in China have contracted the virus as well, according to Chinese officials.
There is some case-by-case decision-making in assessing risk, Rudman said. Whether a health professional was wearing gloves, a mask or other protective equipment, and what kind of interaction they had with the patient, all factor in.
And because they work with people who are sick and may be at higher risk from infection, health care workers may be asked to take more extreme precautions. Santa Clara County’s public health department asked at least five people to go on two weeks of paid leave after a man who visited the hospital where they worked later tested positive for the virus.
Some investigations are easier than others. A coronavirus case recently diagnosed in Wisconsin involved someone who got off a plane from Beijing, went straight to a medical facility while wearing a mask, and has been isolated at home since, according to Public Health Madison & Dane County.
Earlier cases were not so straightforward. One factor that has made the investigations particularly challenging is confusion over whether the virus can be spread by an infected person who is not showing symptoms. Health departments say that, given the uncertainty, they are taking a cautious approach and looking for any contacts going back three days before symptoms started. “Fortunately, we have so few cases, so we can do that,” Rudman said.
Rudman declined to say how many people are being monitored in Santa Clara, but noted that having so few cases has meant she and her colleagues have had time to be methodical about who might be at risk. She hopes that will provide comfort to others in the community.
As for the rest of us, even casual contact with an infected person, such as crossing paths on the street or briefly being in the same room, is thought not to pose much of a risk, though CDC officials stress there is still a lot to learn about the new virus. And the best protection in those instances also can ward off other unwanted visitors this time of year: flu and colds. The latter are often the result of four other coronaviruses that are responsible for a good chunk of winter illnesses.