The federal government in 2020 and 2023 changed who it said could safely donate organs and blood, reducing the restrictions on men who have had sex with another man.
But the FDA’s restrictions on donated tissue, a catchall term encompassing everything from a person’s eyes to their skin and ligaments, remain in place. Advocates, lawmakers, and groups focused on removing barriers to cornea donations, in particular, said they are frustrated the FDA hasn’t heeded their calls. They want to align the guidelines for tissue donated by gay and bisexual men with those that apply to the rest of the human body.
Such groups have been asking the FDA for years to reduce the deferral period from five years to 90 days, meaning a man who has had sex with another man would be able to donate tissue as long as such sex didn’t occur within three months of his death.
One of the loudest voices on lightening the restrictions is Sheryl J. Moore, who has been an advocate since her 16-year-old son’s death in 2013. Alexander “AJ” Betts Jr.’s internal organs were successfully donated to seven people, but his eyes were rejected because of a single question asked by the donor network: “Is AJ gay?”
Moore and a Colorado doctor named Michael Puente Jr. started a campaign called “Legalize Gay Eyes” and together got the attention of national eye groups and lawmakers.

Puente, a pediatric ophthalmologist with the University of Colorado School of Medicine and Children’s Hospital Colorado, said the current patchwork of donor guidelines is nonsensical considering advancements in the ability to test potential donors for HIV.
“A gay man can donate their entire heart for transplant, but they cannot donate just the heart valve,” said Puente, who is gay. “It’s essentially a categorical ban.”
The justification for these policies, set 30 years ago as a means of preventing HIV transmission, has been undercut by the knowledge gained through scientific progress. Now, they are unnecessary and discriminatory in that they focus on specific groups of people rather than on specific behaviors known to heighten HIV risk, according to those who advocate for changing them.
Since 2022, the FDA’s Center for Biologics Evaluation and Research has put changes to the tissue guidance on its agenda but has yet to act on them.
“It is simply unacceptable,” Rep. Joe Neguse (D-Colo.) said in a statement. He was one of dozens of Congress members who signed a letter in 2021 that said the current deferral policies perpetuate stigma against gay men and should be based on individualized risk assessments instead.
“FDA policy should be derived from the best available science, not historic bias and prejudice,” the letter read.
The FDA said in a statement to California Healthline that, “while the absolute risk transmission of HIV due to ophthalmic surgical procedures appears to be remote, there are still relative risks.”
The agency routinely reviews donor screening and testing “to determine what changes, if any, are appropriate based on technological and evolving scientific knowledge,” the statement said. The FDA provided a similar response to Neguse in 2022.
In 2015, the FDA got rid of a policy dubbed the “blood ban,” which barred gay and bisexual men from donating blood, before replacing it in 2023 with a policy that treats all prospective donors the same. Anyone who, in the past three months, has had anal sex and a new sexual partner or more than one sexual partner is not allowed to donate. An FDA study found that, while men who have sex with men make up most of the nation’s new HIV diagnoses, a questionnaire was enough to effectively identify low-risk versus high-risk donors.

The U.S. Public Health Service adjusted the guidelines for organ donation in 2020. Nothing prevents sexually active gay men from donating their organs, though if they’ve had sex with another man in the past 30 days — down from a year — the patient set to receive the organ can decide whether or not to accept it.
But Puente said gay men like him cannot donate their corneas unless they were celibate for five years prior to their death.
He found that, in one year alone, at least 360 people were rejected as cornea donors because they were men who had had sex with another man in the past five years, or in the past year in the case of Canadian donors.
Corneas are the clear domes that protect the eyes from the outside world. They have the look and consistency of a transparent jellyfish, and transplanting one can restore a person’s sight. They contain no blood, nor any other bodily fluid capable of transmitting HIV. Scientists suspect that’s why there are no known cases of a patient contracting HIV from a cornea transplant, even when those corneas came from donors of organs that did infect recipients.
Currently, all donors, whether of blood, organs, or tissue, are tested for HIV and two types of hepatitis. Such tests aren’t perfect: There is still what scientists call a “window period” following infection during which the donor’s body has not yet produced a detectable amount of virus.
But such windows are now quite narrow. Researchers with the Centers for Disease Control and Prevention found that nucleic acid tests, which are commonly used to screen donors, are unlikely to miss someone having HIV unless they acquired it in the two weeks preceding donation. Another study estimated that even if someone had sex with an HIV-positive person a couple of weeks to a month before donating, the odds are less than 1 in a million that a nucleic acid test would miss that infection.
“Very low, but not zero,” said Sridhar Basavaraju, who was one of the researchers on that study and directs the CDC’s Office of Blood, Organ, and Other Tissue Safety. He said the risk of undetected hepatitis B is slightly higher “but still low.”
At least one senior FDA official has indirectly agreed. Peter Marks, who directs the FDA’s Center for Biologics Evaluation and Research, co-authored a report last year that said “three months amply covers” the window period in which someone might have the virus but at levels too low for tests to pick up. Scott Haber, director of public health advocacy at the American Academy of Ophthalmology, said his group’s stance is that the tissue donation guideline “should be at least roughly in alignment” with that for blood donations.
Kevin Corcoran, who leads the Eye Bank Association of America, said the five-year abstinence required of corneal donors who are gay or bisexual isn’t just “badly out of date” but also impractical, requiring grieving relatives to recall five years of their loved one’s sexual history.
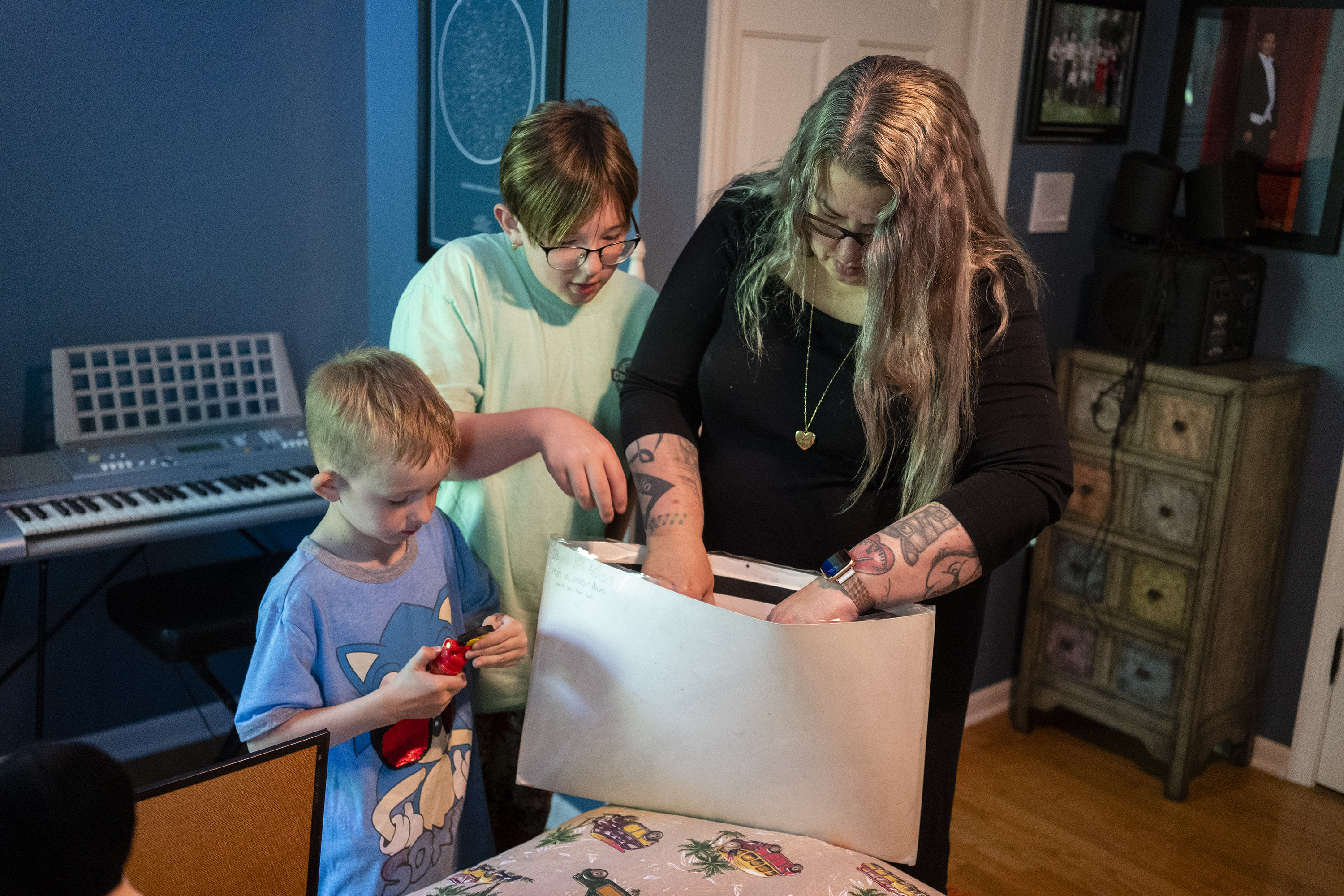
That’s the situation Moore found herself in on a July day in 2013.
Her son loved anime, show tunes, and drinking pop out of the side of his mouth. He was bad at telling jokes but good at helping people: Betts once replaced his little sister’s lost birthday money with his own savings, she said, and enthusiastically chose to be an organ donor when he got his driver’s license. Moore remembered telling her son to ignore the harassment by antigay bigots at school.
“The kids in show choir had told him he’s going to hell for being gay, and he might as well just kill himself to save himself the time,” she recalled.
That summer, he did. At the hospital, as medical staff searched for signs of brain activity in the boy before he died, Moore found herself answering a list of questions from Iowa Donor Network, including, she recalled: “Is AJ gay?”


“I remember very vividly saying to them, ‘Well, what do you mean by, “Was he gay?” I mean, he’s never had penetrative sex,’” she said. “But they said, ‘We just need to know if he was gay.’ And I said, ‘Yes, he identified as gay.’”
The Iowa Donor Network said in a statement that the organization can’t comment on Moore’s case, but said, “We sincerely hope for a shift in FDA policy to align with the more inclusive approach seen in blood donation guidelines, enabling us to honor the decision of all individuals who want to save lives through organ and tissue donation.”
Moore said her son’s organs helped save or prolong the lives of seven other people, including a boy who received his heart and a middle-aged woman who received his liver. Moore sometimes exchanges messages with her on Facebook.
She found out a year later that her son’s corneas were rejected as donor tissue because of that conversation with Iowa Donor Network about her son’s sexuality.
“I felt like they wasted my son’s body parts,” Moore said. “I very much felt like AJ was continuing to be bullied beyond the grave.”
This article was produced by KFF Health News, a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.



