BALTIMORE — Keyonta Parnell has had asthma most of his young life, but it wasn’t until his family moved to the 140-year-old house here on Lemmon Street two years ago that he became one of the health care system’s frequent customers.
“I call 911 so much since I’ve been living here, they know my name,” said the 9-year-old’s mother, Darlene Summerville, who calls the emergency medical system her “best friend.”
Summerville and her family live in the worst asthma hot spot in Baltimore: ZIP code 21223, where decrepit houses, rodents and bugs trigger the disease and where few community doctors work to prevent asthma emergencies. One mom there wields a BB gun to keep rats from her asthmatic child.
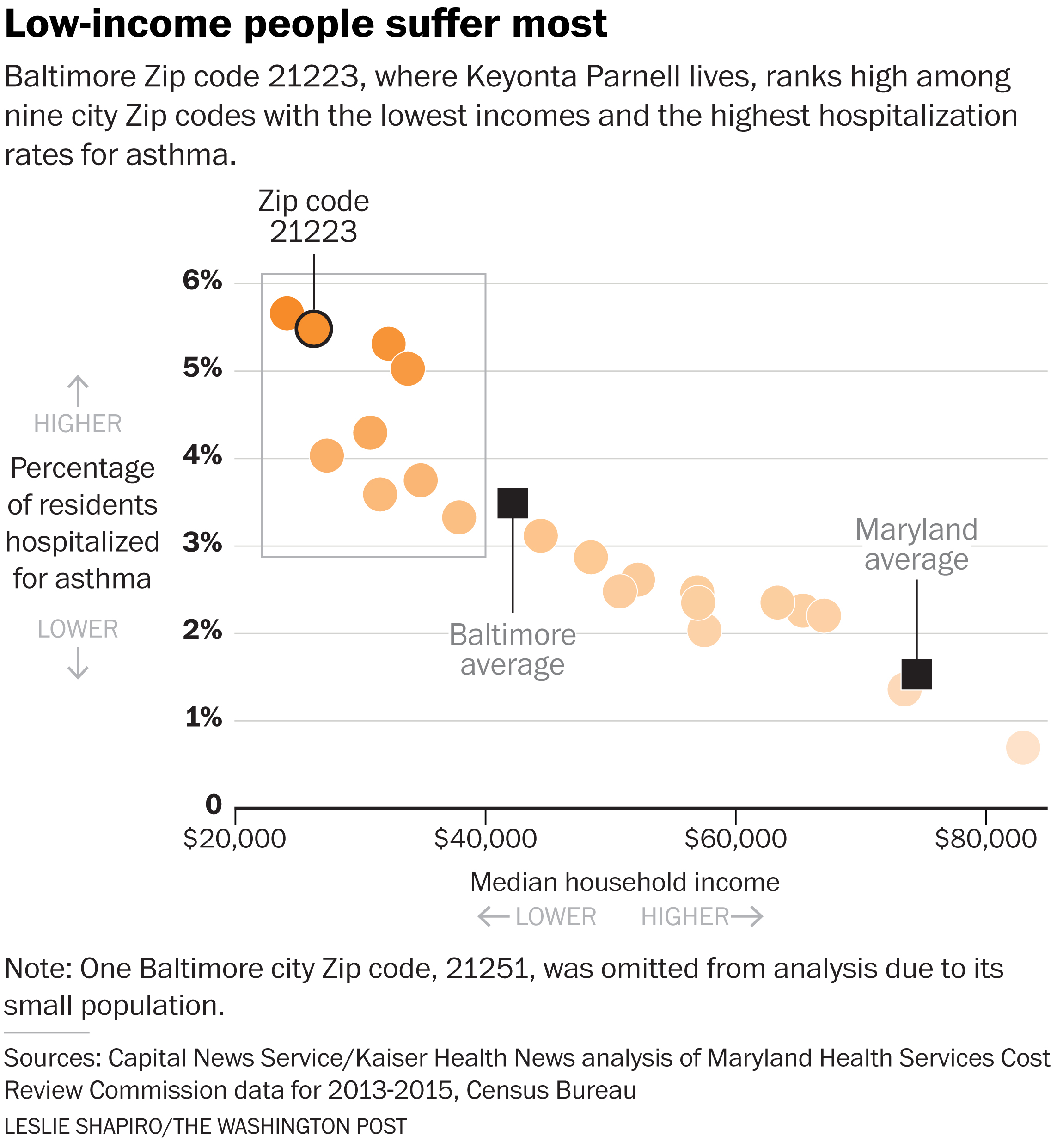
Residents of this area visit hospitals for asthma flare-ups at more than four times the rate of people from the city’s wealthier neighborhoods, according to data analyzed by Kaiser Health News and the University of Maryland’s Capital News Service.
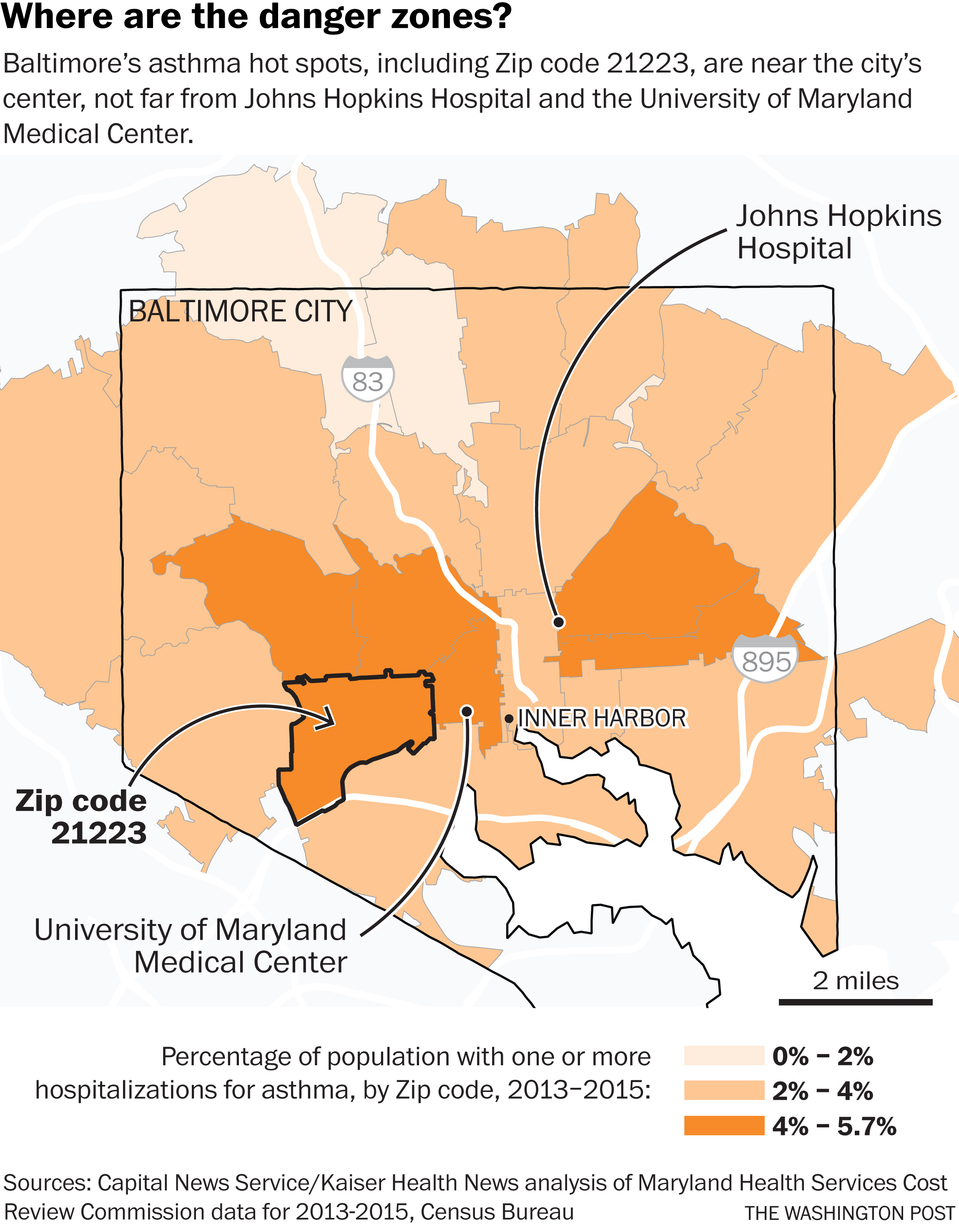 Baltimore paramedic crews make more asthma-related visits per capita in 21223 than anywhere else in the city, according to fire department records. It is the second-most-common ZIP code among patients hospitalized for asthma, which, when addressed properly, should never require emergency visits or hospitalization.
Baltimore paramedic crews make more asthma-related visits per capita in 21223 than anywhere else in the city, according to fire department records. It is the second-most-common ZIP code among patients hospitalized for asthma, which, when addressed properly, should never require emergency visits or hospitalization.
The supreme irony of the localized epidemic is that Keyonta’s neighborhood in southwest Baltimore is in the shadow of prestigious medical centers — Johns Hopkins, whose researchers are international experts on asthma prevention, and the University of Maryland Medical Center.
Both receive massive tax breaks in return for providing “community benefit,” a poorly defined federal requirement that they serve their neighborhoods. Under Maryland’s ambitious effort to control medical costs, both are supposed to try to improve residents’ health outside the hospital and prevent admissions.
But like hospitals across the country, the institutions have done little to address the root causes of asthma. The perverse incentives of the health care payment system have long made it far more lucrative to treat severe, dangerous asthma attacks than to prevent them.
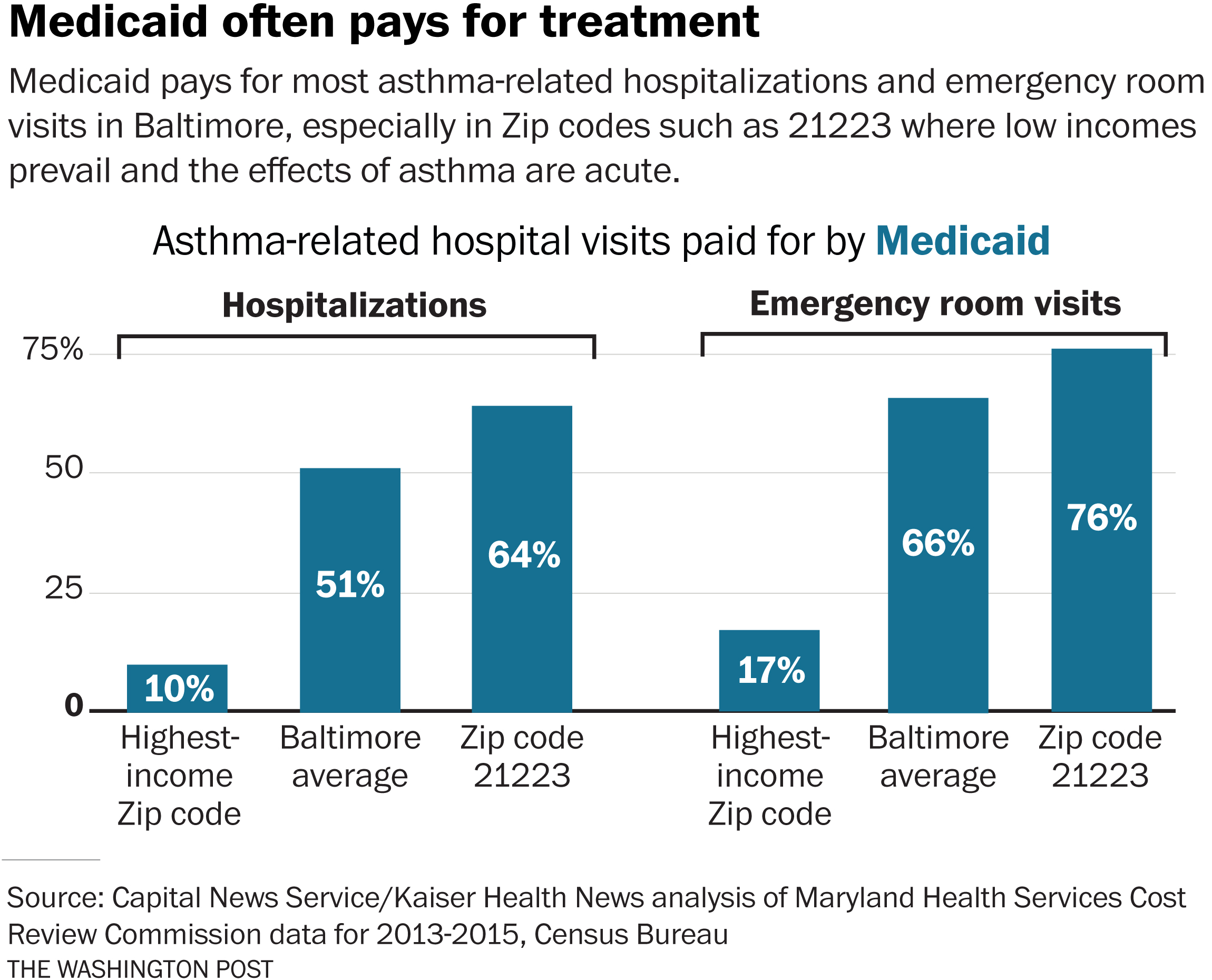
Hopkins, UMMC and other hospitals collected $84 million over the three years ending in 2015 to treat acutely ill Baltimore asthma patients as inpatients or in emergency rooms, according to the news organizations’ analysis of statewide hospital data. Hopkins and a sister hospital received $31 million of that.
Executives at Hopkins and UMMC acknowledge that they should do more about asthma in the community but note that there are many competing problems: diabetes, drug overdoses, infant mortality and mental illness among the homeless.
Science has shown it’s relatively easy and inexpensive to reduce asthma attacks: Remove rodents, carpets, bugs, cigarette smoke and other triggers. Deploy community doctors to prescribe preventive medicine and health workers to teach patients to use it.

Research showing that removing household triggers reduces asthma attacks “is unequivocal,” says Ben Carson, a former Johns Hopkins neurosurgeon and now secretary of the Department of Housing and Urban Development. “The cost of not taking care of people is probably greater than the cost of taking care of them.” (Katherine Gilyard/KHN)
Ben Carson, secretary of the Department of Housing and Urban Development, who saw hundreds of asthmatic children from low-income Baltimore during his decades as a Hopkins neurosurgeon, said that the research on asthma triggers is unequivocal. “It’s the environment — the moist environments that encourage the mold, the ticks, the fleas, the mice, the roaches,” he said in an interview.
As the leader of HUD, he says he favors reducing asthma risks in public housing as a way of cutting expensive hospital visits. The agency is discussing ways to finance pest removal, moisture control and other remediation in places asthma patients live, a spokeswoman said.
“The cost of not taking care of people is probably greater than the cost of taking care of them” by removing triggers, Carson said, adding, “It depends on whether you take the short-term view or the long-term view.”
The Long View
Asthma is the most common childhood medical condition, with rates 50 percent higher in families below the poverty line, who often live in run-down homes, than among kids in wealthier households. The disease causes nearly half a million hospital admissions in the United States a year, about 2 million visits to the emergency room and thousands of deaths annually.
That drives the total annual cost of asthma care, including medicine and office visits, well over $50 billion.
Keyonta lives in a two-bedroom row house on the 1900 block of Lemmon Street, which some residents call the “Forgetabout Neighborhood,” about a mile from UMMC and 3 miles from Hopkins.
Reporters spent months interviewing patients and parents and visiting homes in 21223, a multiracial community where the average household income of $38,911 is lower than in all but two other ZIP codes in Maryland.
To uncover the impact of asthma, the news organizations analyzed every Maryland inpatient and emergency room case over more than three years through a special agreement with the state commission that sets hospital rates and collects such data. The records did not include identifying personal information.
For each emergency room visit to treat Baltimore residents for asthma, according to the data, hospitals were paid $871, on average. For each inpatient case, the average revenue was $8,698. In one recent three-year period, hospitals collected $6.1 million for treating just 50 inpatients, the ones most frequently ill with asthma, each of whom visited the hospital at least 10 times.

Lemmon Street’s trash piles and vacant homes harbor rodents and insects that can set off asthma flare-ups. (Doug Kapustin for KHN)

Darlene Summerville partly blames a moldy dirt basement for triggering her children’s asthma flare-ups. (Doug Kapustin for KHN)
Hopkins’ own research shows that shifting dollars from hospitals to Lemmon Street and other asthma hot spots could more than pay for itself. Half the cost of one admission — a few thousand dollars — could buy air purifiers, pest control, visits by community health workers and other measures proven to slash asthma attacks and hospital visits by frequent users.
“We love” these ideas, and “we think it’s the right thing to do,” said Patricia Brown, a senior vice president at Hopkins in charge of managed care and population health. “We know who these people are. . . . This is doable, and somebody should do it.”
But converting ideas to action hasn’t happened at Hopkins or much of anywhere else.
One of the few hospitals making a substantial effort, Children’s National Health System in Washington, D.C., has found that its good work comes at a price to its bottom line.
Children’s sends asthma patients treated in the emergency room to follow-up care at a clinic that teaches them and their families how to take medication properly and remove home triggers. The program, begun in the early 2000s, cut emergency room use and other unscheduled visits by those patients by 40 percent, a study showed.
While recognizing that it decreases potential revenue, hospital managers fully support the program, said Dr. Stephen Teach, the pediatrics chief who runs it.
“‘Asthma visits and admissions are down again, and it’s all your fault!’” Children’s chief executive likes to tease him, Teach said. “And half his brain is actually serious, but the other half of his brain is celebrating the fact that the health of the children of the District of Columbia is better.”

The Close-Up View
Half of the 32 row houses on Summerville’s block of Lemmon Street are boarded up, occupied only by the occasional heroin user. At least 10 people on the block had asthma late last year, according to interviews with residents then.
“We have mold in our house” and a leaky roof, said Tracy Oates, 42, who lived across the street from Summerville. “That is really big trouble as far as triggering asthma.”
Two of her children have the disease. “I don’t even want to stay here,” she said. “I’m looking for a place.”
Shadawnna Fews, 30, lived with her asthmatic toddler on Stricker Street, a few blocks east. She kept a BB gun to pick off rats that doctors said can set off her son’s wheezing.
Delores Jackson, 56, who lived on Wilkens Avenue, a few blocks south of Lemmon Street, said she had been to the hospital for asthma three times in the previous month.
All three of Summerville’s kids have asthma. Before moving to Lemmon Street two years ago, she remembers, Keyonta’s asthma attacks rarely required medical attention.
But their new house contained a clinical catalog of asthma triggers.
The moldy basement has a dirt floor. Piles of garbage in nearby vacant lots draw vermin: mice, which are among the worst asthma triggers, along with rats. Summerville, 37, kept a census of invading insects: gnats, flies, spiders, ants, grasshoppers, “little teeny black bugs,” she laughed.
Often she smokes inside the house.
The state hospital data show that about 25 Marylanders die annually from acute asthma, their airways so constricted and blocked by mucus that they suffocate.
Keyonta missed dozens of school days last year because of his illness, staying home so often that Summerville had to quit her cooking job to care for him. Without that income, the family nearly got evicted last fall and again in January. The rent is $750.
About a third of Baltimore high school students report they have had asthma, causing frequent absences and missed learning, said Dr. Leana Wen, Baltimore’s health commissioner.
With numbers like that, West Baltimore’s primary care clinics, which treat a wide range of illnesses, are insufficient, as is the city health department’s asthma program, whose three employees visit homes of asthmatic children to demonstrate how to take medication and reduce triggers.
The program, which an analysis by Wen’s office showed cut asthma symptoms by 89 percent, “is chronically underfunded,” she said. “We’re serving 200 children [a year], and there are thousands that we could expand the program to.”
‘The Hospital Instead Of The Classroom’
The federal government paid for $1.3 billion in asthma-related research over the past decade, of which $205 million went to Hopkins, records show. The money supports basic science as well as many studies showing that modest investments in community care and home remediation can improve lives and save money.
“Getting health care providers to pay for home-based interventions is going to be necessary if we want to make a dent in the asthma problem,” said Patrick Breysse, a former Hopkins official, who as director of the National Center for Environmental Health at the Centers for Disease Control and Prevention is one of the country’s top public health officials.
Other factors can trigger asthma: outdoor air pollution and pollen, in particular. But eliminating home-based triggers could reduce asthma flare-ups by 44 percent, one study showed.
Perhaps no better place exists to try community asthma prevention than Maryland. By guaranteeing hospitals’ revenue each year, the state’s unique rate-setting system encourages them to cut admissions with preventive care, policy authorities say.
But Hopkins, UMMC and their corporate parents, whose four main Baltimore hospitals together collect some $5 billion in revenue a year, have so far limited their community asthma prevention to small, often temporary efforts, often financed by somebody else’s money.
UMMC’s Breathmobile program, which visits Baltimore schools dispensing asthma treatment and education, depends on outside grants and could easily be expanded with the proper resources, said its medical director, Dr. Mary Bollinger. “The need is there, absolutely,” she said.
 Hopkins runs “Camp Superkids,” a weeklong, sleep-away summer session for children with asthma that costs participants $400, although it awards scholarships to low-income families. It’s also conducting yet another study — testing referral to follow-up care for emergency room asthma patients, which Children’s National long ago showed was effective.
Hopkins runs “Camp Superkids,” a weeklong, sleep-away summer session for children with asthma that costs participants $400, although it awards scholarships to low-income families. It’s also conducting yet another study — testing referral to follow-up care for emergency room asthma patients, which Children’s National long ago showed was effective.
But no hospital has invested substantially in home remediation to eliminate triggers, a proven strategy supported by the HUD secretary and promoted by Green and Healthy Homes Initiative, a Baltimore nonprofit that works to reduce asthma and lead poisoning.
“We either go forward to do what has been empirically shown to work, or we continue to bury our heads in the sand and kids will continue to go to the hospital instead of the classroom,” said Ruth Ann Norton, the nonprofit’s chief executive.
Hopkins and UMMC say they do plenty to earn their community benefit tax breaks.
“It’s always a challenge to say, ‘Where do we start first?’” said Dana Farrakhan, a senior vice president at UMMC whose duties include community health improvement.
Among other initiatives, UMMC takes credit for working with city officials to sharply reduce infant mortality by working with expectant mothers. The organization’s planned outpatient center will include health workers to help people reduce home asthma triggers, Farrakhan said.
“What we do is perhaps not sufficiently focused,” Brown of Hopkins said. At the same time, “we have to have revenue,” she said. “We’re a business.”
After months of waiting, Summerville considered herself lucky to get an appointment with the city health department’s asthma program.
One of its health workers came to the house late last year. She supplied mousetraps and mattress and pillow covers to control mites and other triggers. She helped force Summerville’s landlord to fix holes in the ceiling and floor.
She urged Summerville to stop smoking inside and gave medication lessons, which uncovered that Summerville had mixed up a preventive inhaler with the medicine used for Keyonta’s flaring symptoms.
“The asthma lady taught me what I needed to know to keep them healthy,” Summerville said of her family.
That was late in 2016. Since then, Summerville said last month, she hasn’t called an ambulance.
Naema Ahmed, Helen Lyons and Talia Richman of Capital News Service and Douglas Birch contributed to this report. Trielli also reports for Capital News Service.
METHODOLOGY:
Kaiser Health News and the University of Maryland’s Capital News Service obtained data held by the Maryland Health Services Cost Review Commission on every hospital inpatient and emergency room case in the state from mid-2012 to mid-2016 — some 10 million cases. The anonymized data did not include identifying personal information.
The news organizations measured asthma costs by calculating total charges for cases in which asthma was the principal diagnosis. Maryland’s hospital rate-setting system ensures that such listed charges are very close to equaling the payments collected.
To determine asthma prevalence, reporters calculated the per capita rate of hospital visits with asthma as a principal diagnosis — a method frequently used by health departments and researchers. This may exaggerate asthma prevalence in low-income ZIP codes such as 21223, because of those communities’ tendency to use hospital services at greater rates.
However, the data also point to high asthma rates in 21223 and other low-income Baltimore communities — for example, asthma prevalence within the population of all hospital patients in a ZIP code.
This story was produced by Kaiser Health News, an editorially independent program of the Kaiser Family Foundation.



