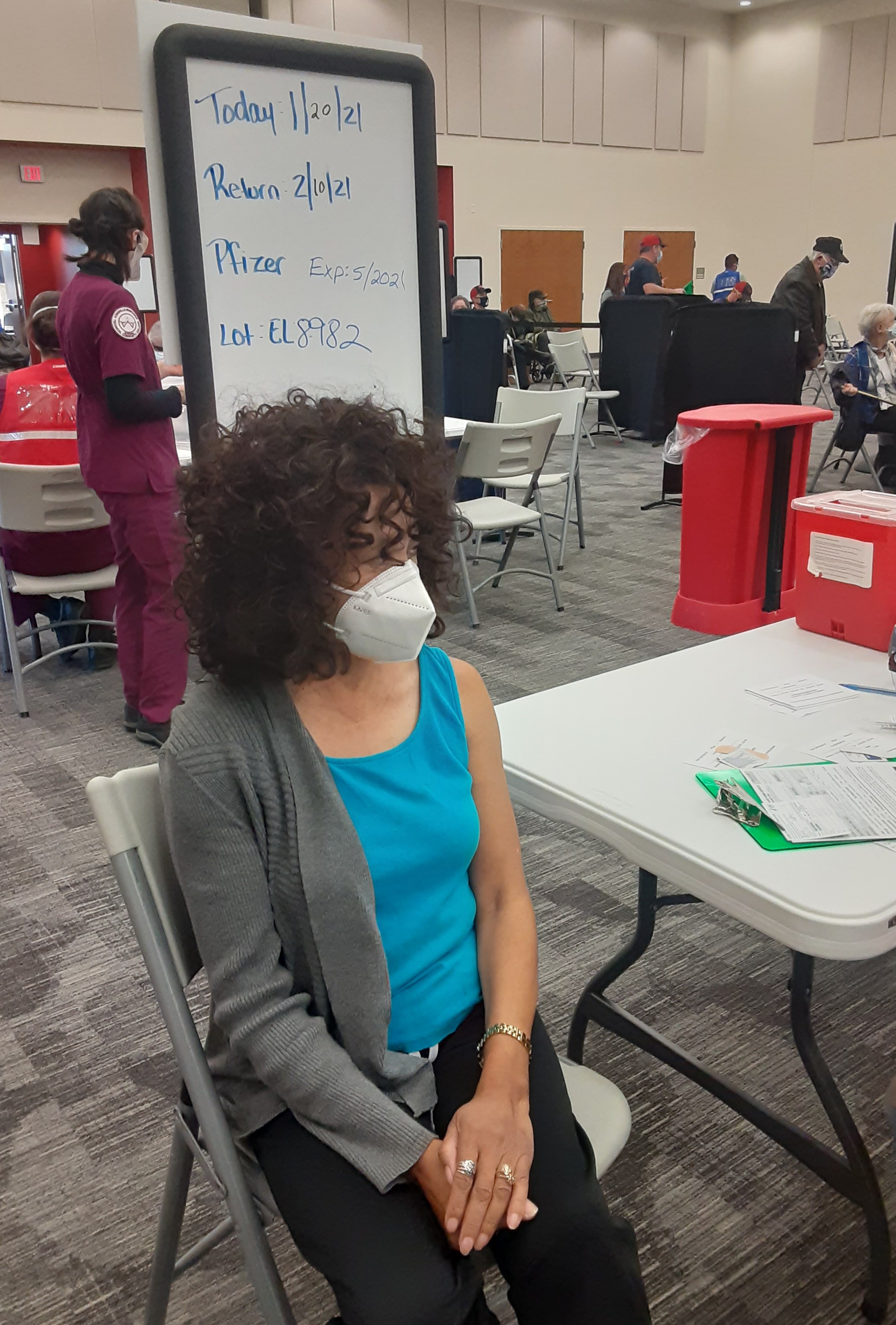
Kim Wagenaar has been preparing to bring covid-19 vaccines to western North Carolina for months.
She’s signed up the community health center she operates in Asheville to receive and distribute the doses. She’s ordered a subzero freezer to store the Pfizer-BioNTech vaccine and transport it to rural counties. She’s also allocated her staff between covid testing sites and vaccine clinics.
But those logistics make up only half the equation, said Wagenaar, CEO of Western North Carolina Community Health Services.
Because the vaccines have a limited shelf life, “you want to make sure you’re ordering what you think you’ll be able to give,” she said. “That’s where messaging comes in.”
While many of the health center’s patients are eager to get their shots, Wagenaar said, she’s worried about other populations in the region — from communities of color to migrant farmworkers and people who live on the street — who may be reluctant to be vaccinated, even though they are more likely to contract the virus.
“It’s so important in this time to go beyond our normal education to reach more communities,” she said.
The concerns arising in western North Carolina, a region tucked between Asheville to the east and the Appalachian Mountains to the west, provide a window into the challenges facing health workers across the country. Not only do they have to transport the vaccine to vulnerable populations, but they also must address those individuals’ concerns and encourage them to take the shots.
Polls show Black and Hispanic Americans, as well as residents of rural areas, have expressed greater reluctance about the vaccine. And disparities in vaccination rates are already emerging.
Now, a host of grassroots organizations in western North Carolina are taking to the streets, to WhatsApp chats and to Zoom lunches to close that gap.
‘You Can Be a Community Hero’
When Adrienne Sigmon talks to people living on the street in Asheville about covid vaccines, she doesn’t suggest the medical system is trying to help them.
As someone who was unsheltered for two years, she knows mistrust of health workers runs deep. Many people who are homeless receive poor care or no care at all.
Instead, Sigmon frames the vaccine as an opportunity to help society. “By getting vaccinated, you can be a community hero,” she tells them.
“Giving people that ownership and sense that they can help in this small way is empowering,” she said.
That’s how Sigmon felt four years ago when she joined the street medic team at BeLoved Asheville, a nonprofit that tackles issues like homelessness and hunger. The team trains people who are currently or formerly unsheltered in basic medical skills, from first aid to wound care and overdose prevention.
“Instead of other people coming in to say, ‘I’m going to fix you and serve you,’ we learn to take care of ourselves and the community,” said Sigmon, who is now a lead street medic.
On Mondays and Thursdays, Sigmon and her team travel through downtown Asheville and the rural corners of Buncombe County to hand out lifesaving supplies like insulated tents, sleeping bags, thermal socks, face masks and hand sanitizer to those living outdoors. Now they also pass out flyers about the vaccines and ask people if they’ll pledge to get their shots.
Some refuse, Sigmon said. They may suffer from mental illness, not believe covid is real or not care if they get sick.
But more often, people have questions: Will I get sick if I get a vaccine? Is it safe, since it came out so quickly?
Sigmon assures them that the vaccines don’t contain the coronavirus and that, although the development process was quick, it built on a decade of research.
Of the hundreds of people Sigmon and her team have spoken with, about 75% have agreed to be vaccinated.

‘Think About Your Older Roommates’
Migrant farmworkers begin arriving in western North Carolina in February, when they work in greenhouses, and stay through the fall or early winter, harvesting crops and Christmas trees.
This past year, conversations about covid vaccines began in July, said Jessica Rodriguez, outreach coordinator for Vecinos Farmworker Health Program, which provides medical services to about 500 migrant workers in the region.
At the time, covid outbreaks across two farms sickened nearly 100 men. “When will this be over?” the workers asked her.
Since then, Rodriguez and her team have been updating the farmworkers about the vaccines.
Men in their 50s and 60s have generally been eager, Rodriguez said. But the younger workers, some just 18 years old, have been hesitant. They’ve received conflicting messages about the seriousness of the virus from family back home, and sometimes from their home countries’ governments.
“Think about your older roommates,” Rodriguez tells them in Spanish. The workers live in tight quarters, often old converted hotels tucked behind a main road or cabins perched on the side of a mountain, with anywhere from five to 50 men together.
“You could get covid and feel nothing at all,” Rodriguez said, “but if you pass it to someone who is older or has diabetes, he could end up in the hospital.”
Rodriguez also posts fact sheets in Spanish on her WhatsApp story, where anyone with her phone number can view them. That’s been particularly popular, she said. Since the workers’ schedules rarely allow them to check for health advisories from the White House or watch the state health secretary’s afternoon telecasts, updates from Rodriguez and her team have been crucial. Even workers she met a few years ago who now live in other countries have messaged her to say thanks for the information on WhatsApp.
Her team also provides in-person education at the camps, where they often bring food and medical supplies.
“As soon as we’d arrive, the whole crew would come out,” she said. “Some of our covid education sessions went up to an hour because the guys had so many questions.”

‘You All Are My Ambassadors’
Kathey Avery, a community health nurse, has been hosting monthly lunch-and-learn meetings for a group of 14 women for nearly a decade.
The youngest attendee is in her 50s, and the oldest is 94. Most are Black women who go to church, volunteer in the community and are in regular contact with their extended families, said Avery, who also co-chairs the Institute for Preventive Healthcare and Advocacy, a grassroots organization that addresses health disparities in Buncombe County.
“Whenever I need to get information out, I tell them, ‘You all are my ambassadors,’” said Avery, who is Black too. “That always makes them smile.”
In the past, Avery talked to them about topics like chronic disease and nutrition. During the pandemic, she’s moved the lunch-and-learns to Zoom and talks about covid symptoms, testing and, now, vaccines.
Black people’s history of mistreatment in the U.S. makes the vaccines a tough sell, Avery said. Many worry about a repeat of the infamous Tuskegee trial, in which Black patients with syphilis were purposely left untreated. Others point to the brutal response to Black Lives Matter protests and efforts to suppress Black votes.
That’s why education about the vaccines has to come from a place they trust, Avery said.
She tries to keep it simple, using a one-page document she created with answers to questions like “What is the definition of ‘vaccine’?” and “What is the definition of ‘virus’?”
It’s a matter of homing in on a couple of points and relating it to “something you know they already know,” Avery said.
Then you build on that knowledge in a second conversation, and a third and fourth.
“If you’re not talking to people and building trust over time,” Avery said, “they won’t listen.”
This story was produced by Kaiser Health News, an editorially independent program of the Kaiser Family Foundation.
[Correction: This article was updated at 11:30 a.m. PT on Feb. 22, 2021, to correct the name of the grassroots organization Kathey Avery helps lead in Buncombe County, North Carolina, to address health disparities.]



