The atmosphere inside the Allen House is easygoing as residents circulate freely through the hallways, meet in group sessions, or gather on a large outdoor patio that features a dirt volleyball court with an oversize net.
The 60-bed safety-net residential treatment center in Santa Fe Springs, run by Los Angeles Centers for Alcohol and Drug Abuse, has a dedicated detox room, on-site physicians and nurses, substance abuse counselors, licensed therapists, and other practitioners. It offers group counseling as well as individual and family therapy, and it endorses the use of medications for addiction treatment, such as buprenorphine and naltrexone, which are increasingly considered the gold standard.
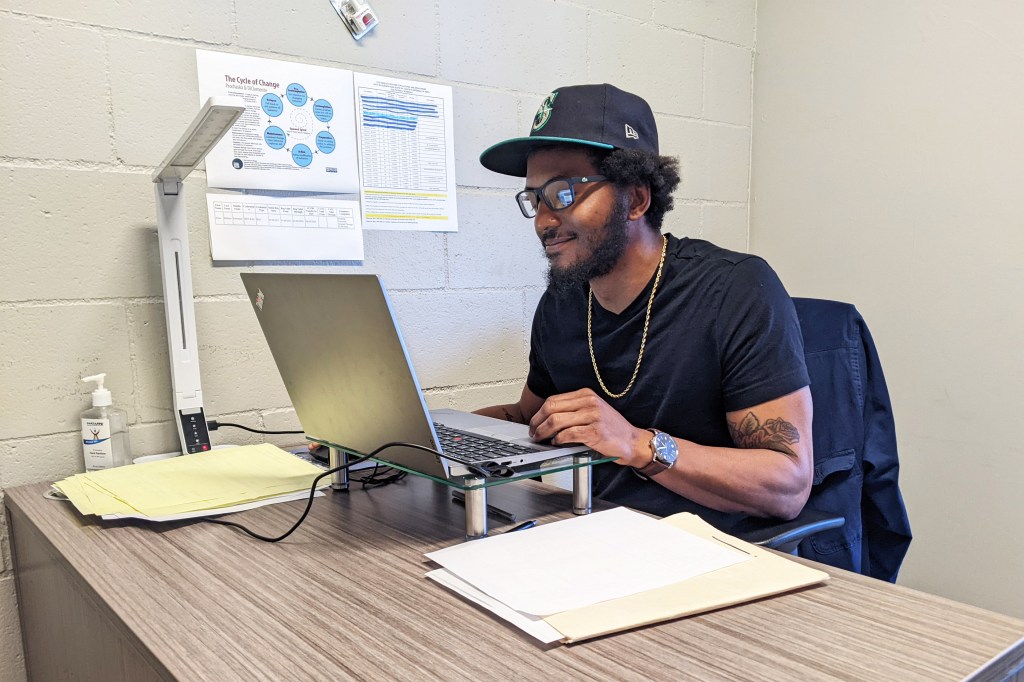
Willard Sexton, a staff member and former Allen House patient, says the most important part of his job is speaking with each resident daily. Most of them, like him, came to treatment straight from jail or prison, and he knows as well as anybody how stressful it is to stop using.
“It’s similar to grief and loss,” says Sexton, 35. “The drug was their best friend for a long time.” Interacting with them, he says, helps him in his own ongoing recovery.
At a time when drug use is among the nation’s gravest public health crises, a visit to the Allen House offers key lessons: Addiction is a chronic illness requiring constant vigilance, there’s no one-and-done solution, and relapses are part of the journey to recovery. Peer mentoring is an invaluable element of drug counseling, since people who have plodded the difficult path from dependence to sobriety understand the mindset of patients on a visceral level.
And most importantly for those who feel despair in the grip of addiction, there is hope. “Recovery happens,” says Michelle Doty Cabrera, executive director of the County Behavioral Health Directors Association of California. “Every single day people come into treatment and succeed in addressing their substance use disorders.”
Drug-related overdoses kill almost as many Californians as lung cancer, more than diabetes, and two to three times as many as car accidents, according to a report by California Health Policy Strategies, a Sacramento consulting group. The report showed there were about 11 times as many fentanyl-related deaths in 2021 as in 2017, accounting for more than half of overdose fatalities. And addiction can ruin lives even if it doesn’t end them.
But proper care for substance use disorders can still be hard to find. Experts in the field say residential treatment beds are in short supply. A pandemic-driven shortage of health care workers has hit the drug treatment world. Unscrupulous operators, with an eye on their bottom lines, may take advantage of people desperate for any answer. Commercial insurers often deny treatment requests or propose cheaper alternatives.
Some treatment programs shun anti-addiction medications that have proven effective. Physicians, nurse practitioners, and other providers with the requisite training can prescribe these drugs in California, but too few seem willing or able to do so — though that could change now that federal law no longer requires them to get a special waiver.
A page on the website of the Substance Abuse and Mental Health Services Administration (www.samhsa.gov) allows you to find practitioners in your area who treat patients with buprenorphine.
There’s no one-size-fits-all solution for addiction. Treatment can differ depending on the substance — opioids, alcohol, or methamphetamine, for example. And people with substance use problems come from all walks of life: Some are straight off the streets or out of jail or may have serious mental or medical conditions that require additional care. Others may be otherwise healthy with good jobs and insurance. If a clinic tries to sell you on a standardized treatment program, cross the place off your list.
And if someone tells you that after one stint in their program you or a loved one will be drug-free for life, run the other way. For many people, addiction is a chronic condition that ebbs and flows over many years. Too often, patients in the throes of an overdose are revived and then discharged with no follow-up.
“If we talked about treating other chronic illnesses like diabetes or asthma in the same way we often approach treating substance use, people would think we were crazy or would sue the doctor for malpractice,” says Bradley Stein, a psychiatrist and senior physician policy researcher at the Rand Corp.

Finding the treatment that is right for you or a loved one will take legwork.
Whether it should be a residential or outpatient program depends on multiple factors. People who need to be shielded from exposure to a dealer or a toxic domestic situation, require detox, or have mental health or medical conditions on top of their drug use generally are better off in a residential setting, says Randolph Holmes, medical director of the Los Angeles Centers for Alcohol and Drug Abuse. Outpatient settings are more suitable for people with stable lives and better health or those transitioning from residential treatment, he says.
The cost of treatment can vary widely depending on duration and the patient’s circumstances. In some cases, it can reach tens or hundreds of thousands of dollars.
Various websites allow you to search for nearby addiction treatment. The Substance Abuse and Mental Health Services Administration has a treatment locator at www.findtreatment.gov, or you can call its help line at 800-662-HELP (4347). Shatterproof (www.shatterproof.org) is another source for finding treatment. In California, the Department of Health Care Services publishes a list of substance use help lines by county.
If you’re on Medi-Cal, California’s version of the federal Medicaid program for low-income residents, your county is a good place to start. It can point you to several options, at least in more populous areas. Almost all patients with the Los Angeles Centers for Alcohol and Drug Abuse, for example, are Medi-Cal enrollees.
If you have commercial insurance, call your health plan first. Parity laws require insurers to cover substance use treatment, though they often find reasons not to provide the treatment your provider recommends. If your plan denies you treatment you think you need, you can file an appeal. The Department of Managed Health Care (www.dmhc.ca.gov), the state’s primary health plan regulator, has a help line (888-466-2219) that can assist in appealing your case. Or you can do it online. If the department does not regulate your plan, it can steer you in the right direction.
And remember that recovery is a long-term commitment.
When Sexton first started using in his early 20s, his drug of choice was meth. He later started smoking it with heroin and fentanyl mixed in, he says.
Several years ago, Sexton spent 45 days in residential rehab and got clean. Then he started seeing a woman who was addicted to heroin. He thought he’d help her get sober but ended up doing drugs with her instead. He landed in jail for two months, and a judge ordered him back into residential drug treatment.
Sexton says he continues to actively pursue his recovery even as he helps others do the same. “There are bumps in the road, but I feel like I’m in a Range Rover,” he says. “I’m not going to spill my coffee.”