Latest California Healthline Stories
Legislation To End Surprise Medical Bills Has High Public Support — In Both Parties
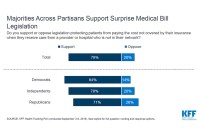
Almost 80% of Americans support efforts in Congress to protect patients from bills that come from doctors or hospitals that were outside their insurance network.
Why Red Wyoming Seeks The Regulatory Approach To Air Ambulance Costs
Wyoming is taking on expensive air ambulance bills by trying to expand Medicaid to cover transport for all patients. This is a big change: a red state seeking to control what’s been a growing free-market bonanza.
Doctors Argue Plans To Remedy Surprise Medical Bills Will ‘Shred’ The Safety Net
A case of questionable logic.
Surprise Medical Bill Legislation Takes A Step Forward, But Will It Lead To A Step Back?
A House committee approved its version of legislation to solve the problem of surprise medical bills. But the measure includes a key provision that’s got less support in the Senate.
Did Your Health Plan Deny You Care? Fight Back.
Most patients don’t argue when their health insurance won’t cover treatment or medication, but they should: Consumers win about half of their appeals. The process can sometimes be overwhelming, but there are ways to prepare and get help.
Hospitals Block ‘Surprise Billing’ Measure
California lawmakers on Wednesday pulled legislation that would have protected some patients from surprise medical bills for emergency care, citing opposition from hospitals. They vowed to resurrect the bill next year.
KHN’s ‘What The Health?’: Dems Debate Health Care
Democratic presidential candidates disagreed on how to fix health care in their first debate Wednesday, although they all called for boosting insurance coverage and lowering prices. Meanwhile, the Trump administration is keeping health care in the news, too, with a new plan to make medical prices more available to the public. Stephanie Armour of The Wall Street Journal, Rebecca Adams of CQ Roll Call and Anna Edney of Bloomberg News join KHN’s Julie Rovner to discuss this, plus the latest in news about bipartisan progress on catch-all legislation to address “surprise” medical bills. Plus, Rovner interviews NPR’s Jon Hamilton about the latest KHN-NPR “Bill of the Month” installment.
Senate Panel Makes Surprisingly Fast Work Of ‘Surprise Medical Bills’ Package
The measure also includes a range of provisions designed to address health care costs.
KHN’s ‘What The Health’: Politics Heading Into 2020: Live From Aspen!
How big an issue will health really be in the 2020 election? Will the Republicans find their political footing on the issue? In this episode of KHN’s “What the Health?” Julie Rovner of Kaiser Health News, Joanne Kenen of Politico and Margot Sanger-Katz of The New York Times report from the Aspen Ideas: Health festival in Aspen, Colo. Joining them are Chris Jennings, who advised Democratic Presidents Bill Clinton and Barack Obama on health policy, and Lanhee Chen, who advised GOP presidential candidates Mitt Romney and Marco Rubio.
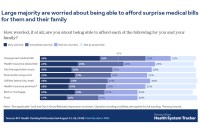
1 In 6 Insured Hospital Patients Get A Surprise Bill For Out-Of-Network Care
On average, 16% of inpatient stays and 18% of emergency visits left a patient with at least one out-of-network charge, most of those came from doctors offering treatment at the hospital, according to a study by the Kaiser Family Foundation.